2025
Altered brain pulsations in phychosis.1Radiology, Oulu University, Oulu, Finland
Synopsis
The detection of functional alterations in psychotic subjects has proven to be a demanding task. In this study we used ultrafast fMRI to investigate physiological brain pulsations driving blood and CSF convection in psychotic brain. We detected dichotomized changes in opposing brain region pulsations between the upper frontal and lower posterior parts of the brain in all three major brain pulsations. The altered brain pulsations in psychotic brains may be connected to abnormal convection of metabolites via CSF and blood providing an physiological basis for the altered reality experiences in psychosis.
INTRODUCTION
Psychosis is a disruptive symptom of several conditions characterized by a loss of ability to differentiate reality from internal mind projections. Recently physiological brain pulsatility measured with fMRI BOLD signal was found to be altered in schizophrenic subjects1,2, suggesting altered convection of metabolites in both CSF and blood3. However, it was unclear which physiological brain pulsation (vasomotor, respiratory or cardiovascular) was affected and where in the brain. In order to figure out how exactly the physiological pulsations are altered in the psychotic state, we used ultrafast fMRI to dissociate the three major brain pulsations without aliasing in order to comprehensively quantify these changes in psychotic subjects.METHODS
After Ethical committee approval and informed consent, 30 psychotic (M/F: 12/16, age 31:22-51 years) subjects and matched healthy ((M/F: 12/16, age 30:20-57 years) controls were scanned with a Siemens Skyra 3T scanner using ultrafast 10 Hz whole brain 3D MREG sequence (TR 100 ms, FA 5°, TE 36 ms, FOV 192 mm3, 3 mm cubic voxel). Routine FSL MELODIC preprocessing pipeline was performed prior to remove scanner warming effects and motion effect. Brains were realigned to MNI space after co-registration with individual T1 3D mprage data. Each brain voxel was calculated into an FFT spectrum using AFNI 3dperiodogram. Individual respiratory belt and SpO2 fingertip reading were used to measure individual cardiorespiratory frequencies and these data were used to calculate individual FFT power at the peak frequency power with a +/- 0.05 Hz band on both sides of the peak. We compared the power of each physiological brain pulsation statistically in psychotic subjects vs. controls with FSL randomise TFCE (p-value threshold p < 0.05, FWE corrected) between the groups. Each pulsation power was also illustrated from tstat group maps.RESULTS
Both the cardiovascular (Fig.1), and, vasomotor (Fig. 2) related pulsations were reduced in the upper frontal regions of the brain. Interestingly, the respiratory pulsation power was significantly increased in the posterior and lower parts of the brain, c.f. Fig 3. As viewed from the sagittal side view, the brain can be divided into opposing areas of increased and decreased physiological pulsations.DISCUSSION
The current results indicate that psychotic subjects have markedly altered brain pulsations driving both CSF and blood flow of the brain arguably altering brain homeostatic balance of substances. The changes occur in primary sensory areas opposing to more frontal cognitive frontal brain structures with a divisional in between. Compared to normal sleep related pulsation changes increasing all pulsations in posterior parts4, the psychotic state seems to add areas of inversely reduced pulsations in the frontal brain areas.CONCLUSION
The results indicate an altered physiological pulsation in psychotic subjects suggesting a more physiological origin for the altered state of reality perception.Acknowledgements
This work was supported by Uniogs/MRC Oulu DP-grant, Pohjois-Suomen Terveydenhuollon tukisäätiö, JAES-Foundation, Academy of Finland and Aivosäätiö TERVA grant 314497, Academy of Finland Grant 275342, The Finnish Medical Foundation, Finnish Neurological Foundation, KEVO grants from Oulu University hospital, Orion Research Foundation, Medical Research Center (MRC) –Oulu, Maire Taponen Foundation, Finnish Brain Foundation, We wish to acknowledge Jussi Kantola for data management and reconstruction of MREG data, the CSC – IT Center for Science Ltd., Finland for generous computational resources.References
1. Saarinen et al, The relationship of genetic susceptibilities for psychosis with physiological fluctuation in functional MRI data Psychiatry Res Neuroimaging 2020, 297:111031. doi: 10.1016/j.pscychresns.2020.111031
2. Saarinen et al., Structural and functional alterations in the brain gray matter among first-degree relatives of schizophrenia patients: A multimodal meta-analysis of fMRI and VBM studies Schizophr Res 2020 216:14-23. doi: 10.1016/j.schres.2019.12.023.
3. Kiviniemi V et al., Ultra-fast magnetic resonance encephalography of physiological brain activity - Glymphatic pulsation mechanisms? JCBFM 2016, 36(6):1033-45.
4. Helakari et al., Sleep-specific changes in physiological brain pulsations. BioRxiv 2020, doi.org/10.1101/2020.09.03.280479
Figures
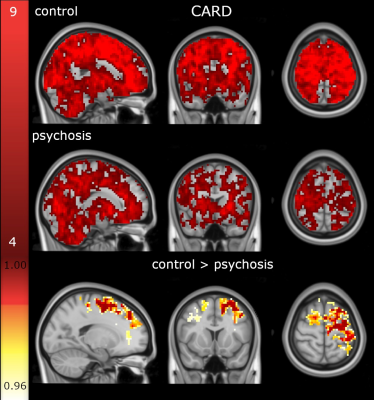
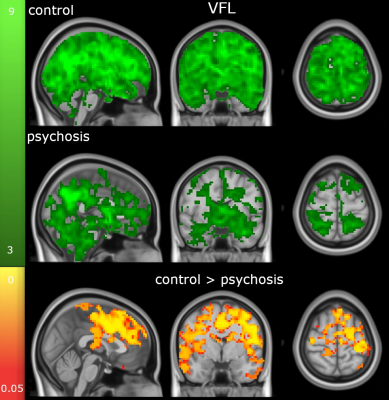
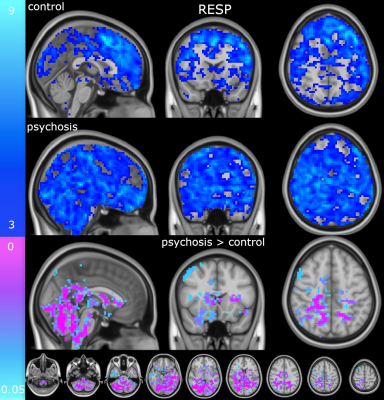
Figure 3. Shows individual respiratory pulsation power maps (z-score > 3) in controls (up), psychotic subjects (middle) and below significant increase in FFT power of psychotic subject brain pulsation (FWE corrected, p < 0.05). The changes oppose those of the decreased pulsations showing up in the posterior occipital, parietal and cerebellar areas quite symmetrically.