1938
Clinical value of MRI-detected extramural vascular invasion in predicting distant metastasis of rectal cancer1Yangpu Hospital, School of Medicine, Tongji University,, shang hai, China, 2Department of Radiology, Yangpu Hospital, Tongji University School of Medicine, Shanghai, shang hai, China, 3Department of General Surgery, Yangpu Hospital, Tongji University School of Medicine, Shanghai, Shanghai, China, 4Department of Radiology, Yangpu Hospital, Tongji University School of Medicine, Shanghai, Shanghai, China, 5MR Scientific Marketing, Diagnostic Imaging, Siemens Healthcare Ltd., Shanghai, Shanghai, China, 6Department of Radiology, Tongji Hospital, Tongji University School of Medicine, Shanghai, Shanghai, China
Synopsis
The results of the present study suggest that there was a significant difference in the occurrence of distant metastasis between RC patients with or without mrEMVI, CRM invasion, regional LN metastasis, and MR peritoneal reflex involvement. And mrEMVI and regional LN metastasis were independent risk factors for distant metastasis of rectal cancer. Therefore, MRI can be used to observe the status of EMVI before surgery, which is helpful for the formulation of individualized treatment plans for rectal cancer and assessment of prognosis.
Purpose
To explore the relationship between extramural vascular infiltration detected by MR and distant metastasis in T3-T4 rectal cancer.Method
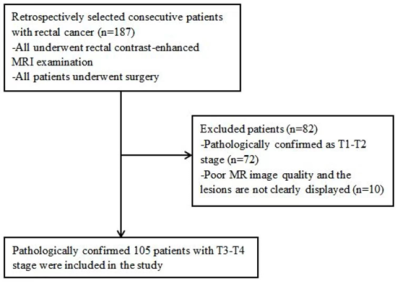
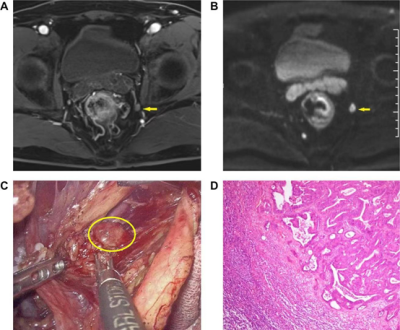
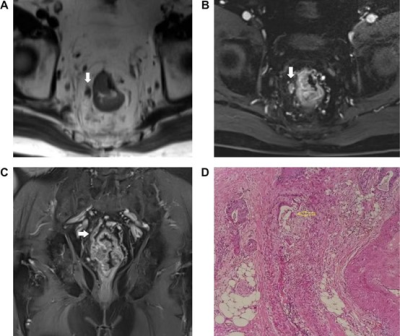
105 patients with pathologically confirmed stage T3-T4 rectal cancer (1) who received surgical treatment between January 2015 and January 2020 were enrolled in this study. Whole pelvic scan was performed using 3T MR (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) with an 18-channel phased array coil. Routine sagittal/axial T2WI and T1WI were as the following parameters: sagittal T2WI (TR= 1000ms, TE= 89ms, matrix= 320×200, FOV= 420mm×420mm), axial T2WI (TR= 1600ms, TE= 96ms, matrix=320×200, FOV= 380×270mm), T1WI (TR=600ms, TE=20ms, matrix= 360×270, FOV=320×260mm). In axial DWI scan, the diffusion-sensitive factor b was set as 0, 50 and 800s/mm2 (TR= 5200ms, TE= 67ms, thickness = 3 mm, matrix = 112×140, FOV= 230×230mm). Enhanced sequence, scanning in three directions of axial, coronal and sagittal T1WI, 3D_vibe sequence were used by injecting the contrast medium GD-DTPA. Analyze the univariate associations of age, gender, MRI and pathological characteristics with distant metastasis and independent risk factors for distant metastasis of rectal cancer.Results
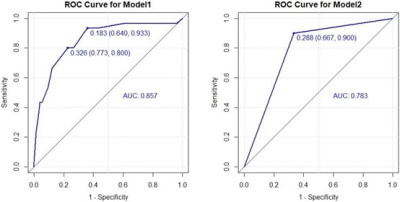
Of the 105 included cases, distance metastasis was confirmed in 30 (28.6%) cases. The incidence of mrEMVI, CRM invasion, regional LN metastasis, and MR peritoneal reflex involvement in the distant metastasis group was higher than that in the non-metastasis group. In the multiple logistic regression model, mrEMVI and regional LN metastasis are independent risk factors for distant metastasis: mrEMVI (OR 16.08), regional LN metastasis (OR 1.80 for N1 vs. N0; OR 8.19 for N2 vs. N0). In addition, according to ROC curves, the diagnostic efficacy of the combination of mrEMVI and regional LN metastasis (sensitivity 0.933, Specificity 0.640, AUC 0.857) is better than mrEMVI alone (sensitivity 0.900, Specificity 0.667, AUC 0.783). Conclusions: mrEMVI and pathological regional LN metastasis are independent risk factors for the distant metastasis of rectal cancer, and the combination of mrEMVI and pathological regional LN metastasis is more effective than mrEMVI alone. As a preoperative prediction program, mrEMVI plays a guiding role in the formulation of treatment programs and the evaluation of prognosis.Conclusion
mrEMVI and pathological regional LN metastasis are independent risk factors for the distant metastasis of rectal cancer, and the combination of mrEMVI and pathological regional LN metastasis is more effective than mrEMVI alone. As a preoperative prediction program, mrEMVI plays a guiding role in the formulation of treatment programs and the evaluation of prognosis.Synopsis
The results of the present study suggest that there was a significant difference in the occurrence of distant metastasis between RC patients with or without mrEMVI, CRM invasion, regional LN metastasis, and MR peritoneal reflex involvement. And mrEMVI and regional LN metastasis were independent risk factors for distant metastasis of rectal cancer. Therefore, MRI can be used to observe the status of EMVI before surgery, which is helpful for the formulation of individualized treatment plans for rectal cancer and assessment of prognosis.Acknowledgements
NoneReferences
1.Singh M, Sircar K, Tandon A, Chowdhry A, Popli DB. The role of tobacco as an etiological agent for oral cancer: Cytomorphometrical analysis of the buccal mucosa in tobacco users. Dent Res J (Isfahan). 2014;11:649-655
2.Khatri VP, Petrelli NJ, Belghiti J. Extending the frontiers of surgical therapy for hepatic colorectal metastases: is there a limit? J Clin Oncol. 2005;23:8490-8499.10.1200/jco.2004.00.6155
3.Peeters KC, Marijnen CA, Nagtegaal ID, et al. The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg. 2007;246:693-701.10.1097/01.sla.0000257358.56863.ce
4.Tripathi P, Rao SX, Zeng MS. Clinical value of MRI-detected extramural venous invasion in rectal cancer. J Dig Dis. 2017;18:2-12.10.1111/1751-2980.12439
5.Zhang XY, Wang S, Li XT, et al. MRI of Extramural Venous Invasion in Locally Advanced Rectal Cancer: Relationship to Tumor Recurrence and Overall Survival. Radiology. 2018;289:677-685.10.1148/radiol.2018172889
6.Horn A, Dahl O, Morild I. Venous and neural invasion as predictors of recurrence in rectal adenocarcinoma. Dis Colon Rectum. 1991;34:798-804.10.1007/bf02051074
7.Bokey EL, Chapuis PH, Dent OF, et al. Factors affecting survival after excision of the rectum for cancer: a multivariate analysis. Dis Colon Rectum. 1997;40:3-10.10.1007/bf02055674
8.NICE. Colorectal cancer: diagnosis and management Clinical guideline [CG131] 2014 [updated 03 December 2014. Available from: https://www.nice.org.uk/guidance/CG131.
9.Talbot IC, Ritchie S, Leighton MH, Hughes AO, Bussey HJ, Morson BC. The clinical significance of invasion of veins by rectal cancer. Br J Surg. 1980;67:439-442.10.1002/bjs.1800670619
Figures