1935
Imaging the hypothalamus in Prader-Willi Syndrome1Department of Psychiatry, University of Cambridge, Cambridge, United Kingdom
Synopsis
Prader-Willi Syndrome (PWS) is a neurodevelopmental disorder characterised by intellectual disability, emotional dysregulation and importantly, marked overeating behaviour. The hypothalamus controls food intake and satiety by endocrine control, and evidence from animal studies has shown that lesions of the hypothalamic nuclei result in hyperphagia. However, studies examining the hypothalamus in humans in vivo are scarce. We show here significantly lower volumes of the hypothalamus and hypothalamic nuclei in PWS compared to healthy controls and general population obese individuals. Our findings are strongly suggestive that impaired appetite control and problematic eating behaviours are a consequence of abnormal hypothalamic structure in PWS.
Body of Abstract
IntroductionPrader-Willi Syndrome (PWS) is a neurodevelopmental disorder caused by the failure of paternal expression of maternally imprinted genes at the chromosomal locus 15q11-13. PWS is characterised by intellectual disability, emotional dysregulation and importantly, marked overeating behaviour which causes obesity and obesity-related conditions, which are a common precursor to premature death. Studies [1, 2] indicate that satiety responses are delayed and transitory in PWS. Neuroimaging research has demonstrated a greatly increased threshold for satiety, reporting greatly reduced or absent satiety responses after large calorie intake [3].
The hypothalamus controls food intake and satiety perception by endocrine control, and evidence from animal studies has shown that lesions of the hypothalamic nuclei result in hyperphagia. However, due to the small size of the hypothalamus and lack of defined image contrast in neuroimaging acquisitions, studies examining its structure and function in humans in vivo are scarce. Here, we apply a recently developed automated tool to segment the hypothalamus in PWS for the first time [4], with the reasoning that disordered hypothalamic development likely plays a critical role in the dysregulation of eating behaviour in PWS.
Methods
Twenty participants with diagnostic confirmation of PWS, forty neurotypical age-matched controls and forty-two obese participants underwent a 3T structural T1-weighted MRI scan acquisition. Obese participants were matched for body mass index (BMI) to the PWS group. The T1 scans were acquired with a TR of 18.7ms, flip angle was 20 degrees, FOV was 256x256mm, with a slice thickness of 1mm, voxel size of 1mm x 1mm and a total of 176 slices. The whole hypothalamus and it’s subnuclei were segmented from the structural acquisitions using an automated tool based on a deep convolutional neural network in FreeSurfer development version 7 [4]. Subnuclei per hemisphere were segmented and identified as the following: anterior-inferior, anterior-superior, posterior, tubular inferior and tubular superior.
The WAIS-IV (Wechsler, 2008) was used to assess IQ in participants with PWS. The Food Related Problem Questionnaire (FRPQ), designed for use in the PWS population, was used to provide information relating to eating behaviour, including subscales for preoccupation with food, satiety impairment and other food-related problem behaviours. Statistical analyses of volumetric quantifications of the hypothalamus, constituent nuclei and behavioural data were performed in R, using Mann-Whitney U between group hypothesis testing and linear regression for associative analyses.
Results
As expected, BMI was significantly higher in the PWS group compared to controls, and IQ was significantly lower in PWS (p < 0.05).
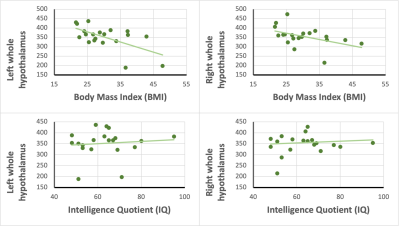
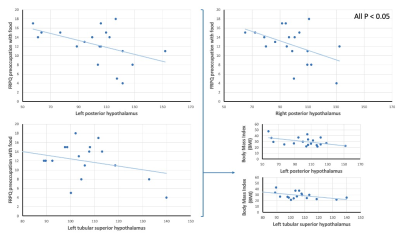
All left hemisphere hypothalamic nuclei were significantly smaller in the PWS group, compared to neurotypical controls (p < 0.01), and all right hemispheric hypothalamic nuclei were significantly smaller in the PWS group (p < 0.01), with the exception of the anterior-inferior nucleus (p = 0.07). Lower whole hypothalamus volume in both hemispheres was significantly associated with increased BMI in PWS (p < 0.05) (Fig.1), but hypothalamus volume was not associated with either IQ or age. Moreover, increased preoccupation with food, as measured by the FRPQ, was seen to be significantly associated with lower volumes of the bilateral posterior nuclei and left tubular superior nucleus. The aforementioned left nuclei also showed significant association between higher BMI and lower volume (Fig. 2).
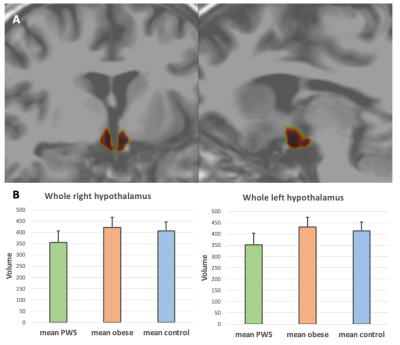
To examine whether the relationship between hypothalamic volume and BMI was driven by the effects of obesity, we then compared the PWS group to neurotypical obese participants. Both the whole hypothalamus bilaterally and all individual nuclei were significantly smaller in PWS compared to obese participants (p < 0.001) (Fig. 3). Additionally, hypothalamic volumes did not differ in any region between the general population obese group and the non-obese controls. Moreover, unlike in the PWS group, obese participants did not show a relationship between hypothalamic volume and BMI in any nuclei.
Discussion
Our primary finding of a significant reduction in size of the hypothalamus and constituent nuclei in PWS compared to controls, and the within PWS group relationship with BMI and preoccupation with food as measured by the FRPQ is strongly suggestive of dysregulation of hypothalamic control of appetite in PWS. Moreover, we established that in an obesity group without neurodevelopmental disorder, matched for BMI to the PWS group, hypothalamic volume was equivalent to healthy controls. We therefore show that abnormal structure and volume of the hypothalamus is not a general consequence or cause of obesity, and that instead, in PWS, hypothalamic dysfunction linked to eating behaviour is neurodevelopmental in nature. Further to this, we posit that early, potentially pre-natal, development of the hypothalamic structures is impaired in PWS, and is a major cause of dysregulated appetite.
Conclusion
We show here significantly lower volumes of the hypothalamus and hypothalamic nuclei in PWS compared to both healthy controls and general population obese individuals. Our findings are strongly suggestive that impaired appetite control and problematic eating behaviours are a consequence of abnormal hypothalamic structure, and that these differences in the hypothalamus are neurodevelopmentally driven.
Acknowledgements
The research was funded by the Prader-Willi Syndrome Association UK (grant number RG63385). KM was supported by the Pinsent Darwin Studentship in Mental Pathology and by St John's College, University of Cambridge. AH received support from the Health Foundation (grant number RG34317) and NIHR Collaborations for Leadership in Applied Health Care Research and Care (CLAHRC) East of England. Funding bodies had no role in the study design, data collection, data analysis, data interpretation, writing of the report or the decision to submit for publication. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
The PWS research programme has also been supported by a generous donation from Jo and Rob Gambi.
References
[1] Zipf, W.B. and G.G. Berntson, Characteristics of abnormal food-intake patterns in children with Prader-Willi syndrome and study of effects of naloxone. Am J Clin Nutr, 1987. 46(2): p. 277-81.2.
[2] Holland, A.J., et al., Measurement of excessive appetite and metabolic changes in Prader-Willi syndrome. Int J Obes Relat Metab Disord, 1993. 17(9): p. 527-32.3.
[3] Hinton, E.C., et al., Neural representations of hunger and satiety in Prader-Willi syndrome. Int J Obes (Lond), 2006. 30(2): p. 313-21.4.
[4] Billot, B., et al., Automated segmentation of the hypothalamus and associated subunits in brain MRI. Neuroimage, 2020. 223: p. 117287.
Figures