1907
Machine learning for detecting intracranial dural arteriovenous fistula on susceptibility weighted image using a convolutional neural network
Bejoy Thomas1, Jithin S S1, Ajimi mol Anzar1, and Santhosh Kannath2
1Imaging Sciences and Interventional Radiology, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram, India, 2Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram, India
1Imaging Sciences and Interventional Radiology, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram, India, 2Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram, India
Synopsis
Artificial intelligence techniques are widely used in medical imaging and diagnostics. In this retrospective study, a convolutional neural network (CNN) architecture was developed to classify intracranial dural arteriovenous fistula (DAVF) on Susceptibility Weighted Images (SWI). The dataset used was a total of 3965 SWI image slices of DAVF patients and 4380 images of controls. The proposed classifier showed significant accuracy in the diagnosis of DAVF and it could be developed as a computer assisted diagnosis tool to identify unsuspected DAVF in routine MR imaging.
Introduction
The natural history and prognosis of intracranial dural arteriovenous fistula (DAVF) is variable and early diagnosis is critical in order to positively impact the clinical course of aggressive (DAVF)1,2. Artificial intelligence (AI) based techniques can be promising in this regard, where these tools can potentially scour the images for possibility of having DAVF and can notify the radiologist or physician about the need for further investigation that can reduce the diagnostic errors and increase the reporting accuracy3,4. In this retrospective study, we proposed a convolutional neural network (CNN) to determine whether intracranial DAVF could be reliably identified on susceptibility-weighted images (SWI).Methods
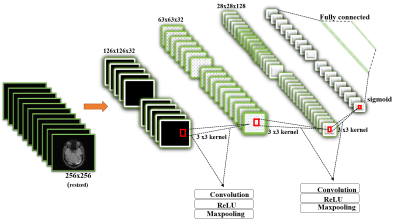
A total of 3965 SWI image slices from 30 angiographically proven DAVF patients and 4380 SWI image slices from 40 age-matched patients with normal MRI findings as control group were included. Proposed CNN architecture is depicted in figure 1. In first experiment, all the images pertaining to the patients were categorised as either DAVF or non-DAVF and the data was trained. Following this, a second experiment was conducted were all the individual labelled slices were trained and in this iteration, a total of 481 labelled DAVF dataset was available. For training and model evaluation, it tool 34 hours for experiment 1 and 12 hours for experiment 2. In the test phase, entire imaging study was fed into the classifier in first approach, while in the second, the particular image set was categorised as DAVF, only if a stack of consecutive pre-required number (2,4,6,8,10 and 12) was positive for the diagnosis.Results
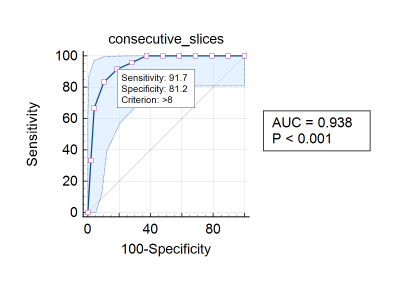
The training process ended in the 20th epoch, with an accuracy of 99.3% for training data and 99.1 % accuracy for validation data. The evaluation of test set demonstrated a classifier accuracy of 67.46%. For the second experiment, the training process achieved a 88% accuracy and validation set reached 89% accuracy. For test set, an accuracy of 83.33% was obtained. Using a prerequisite stack of consecutive positive slices as cut-off for the diagnosis of DAVF (experiment 2), ROC analysis yielded area under the curve of 0.938 (p <0.001). Consecutive positive 6 slices yielded a sensitivity of 100% with improved specificity of 62.5%, while setting 8 slices improved the specificity to above 81.2%, with a marginal decrease of sensitivity to 91.7%. According to this criteria, one transverse dural sinus fistula was mistaken for a normal MR and one normal patient was diagnosed as having DAVF.Discussion
The results of this study are encouraging and comparable to the performance of AI in the detection of other neurovascular diseases. Our results show that CNN can extract discriminative features of SWI slices for the classification of DAVF from normal. CNN models achieve good accuracy in the diagnosis of DAVF with excellent sensitivity and specificity. Such CAD tools can be developed and incorporated in-house and these tools can aid and augment radiology reporting.Conclusion
CNN can extract discriminative features of SWI slices for the classification of DAVF from normal. CNN models achieve good accuracy in the diagnosis of DAVF with excellent sensitivity and specificity.Acknowledgements
Authors acknowledge the grant support of Cognitive Science Research Initiative, Department of Science and Technology, Govt. of India (DST/CSRI/2018/11)References
- Jain N, Kannath S, Kapilamoorthy T, Thomas B. The application of susceptibility-weighted MRI in pre-interventional evaluation of intracranial dural arteriovenous fistulas. J Neurointerv Surg. 2016;9(5):502-507. doi:10.1136/neurintsurg-2016-0123142.
- Reynolds M, Lanzino G, Zipfel G. Intracranial Dural Arteriovenous Fistulae. Stroke. 2017;48(5):1424-1431. doi:10.1161/strokeaha.116.0127843.
- Hosny A, Parmar C, Quackenbush J, Schwartz L, Aerts H. Artificial intelligence in radiology. Nature Reviews Cancer. 2018;18(8):500-510. doi:10.1038/s41568-018-0016-54.
- Duong M, Rauschecker A, Mohan S. Diverse Applications of Artificial Intelligence in Neuroradiology. Neuroimaging Clin N Am. 2020;30(4):505-516. doi:10.1016/j.nic.2020.07.003
DOI: https://doi.org/10.58530/2022/1907