1835
MRI Measures of Non-atherosclerotic Brain Arterial Remodeling in a Population-based Study1Radiology, Johns Hopkins University, Baltimore, MD, United States, 2Joint Department of Biomedical Engineering, University of North Carolina & North Carolina State University, Raleigh, NC, United States, 3Gilman School, Baltimore, MD, United States, 4Radiology, University of Maryland School of Medicine, Balitimore, MD, United States
Synopsis
We have reported reliable MRI measures of non-atherosclerotic brain arterial remodeling (NABAR), as assessed by outward and tortuous remodeling of the large intracranial arteries in older individuals. This will allow us to elucidate the predictors of prevalent and progressing NABAR, and its correlations with brain hypoperfusion and cognition function in an older community-based population.
Introduction
Non-atherosclerotic brain arterial remodeling (NABAR) of large intracranial arteries has recently emerged as a determinant of poor cognitive outcomes1,2. Vascular aging is associated with medical fragmentation and collagen deposition and may present as either outward or tortuous remodeling, both of which may occur in the absence of atherosclerosis3,4. We propose to report the basic characteristics of NABAR, as quantified by luminal diameters and degree of tortuosity, and the reliability for its measurements, in older individuals from a general population.Methods
1,980 Atherosclerosis Risk in Communities (ARIC) study participants who underwent brain MRI from 2011 to 2013 were included in this study. All brain MRI exams were acquired on 3.0 T Siemens scanners using a standardized protocol including a 3D time-of-flight (TOF) MRA sequence. 102 participants returned for repeat MRI exams to estimate scan and reader variability. The 3D TOF MRA was acquired in a transverse plane through the circle of Willis, with the following parameters: TR/TE/flip angle, 21 ms/3.7 ms/18°; field of view, 160 mm x160 mm2; matrix, 320 x 320; acquired resolution, 0.50×0.50 mm2; slice thickness 0.55 mm; slice number, 8.3 cm coverage; and scan time of approximately five minutes. Quantitative measurements (lumen area, diameter, and volume) were determined using LAVA software with non-uniform rational b-splines surface modeling with automated centerline segmentation (Figure 1). Tortuosity was calculated as: tortuosity = arc/chord. The arc is the length of the centerline of the vessel segment, and the chord is the straight distance between proximal and distal points, which are derived variables of LAVA output files. Quantitative measurements were obtained at designated vessel segments (supraclinoid internal carotid artery (ICA), M1 segment of the middle cerebral artery (MCA), dominant A1 segment of the anterior cerebral artery (ACA), P1 segment of the posterior cerebral artery (PCA), basilar artery (BA) and dominant V4 segment of the vertebral artery (VA) over a fixed length for all participants (Figure 2). Arterial diameters and tortuosity were further adjusted to the intracranial volume, and presence of intracranial atherosclerosis to account for differences in the head size and effects from the atherosclerotic process, respectively. Reliability was assessed by person correlation.Results
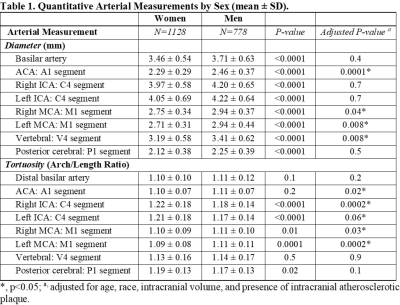
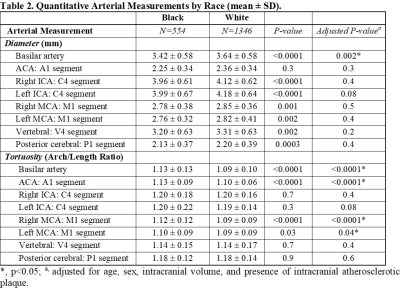
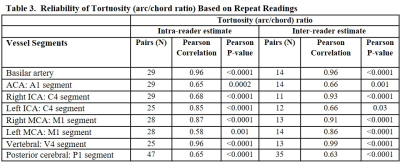
A total of 1,906 participants (age 67-90 years; 1,128 women; 554 black) had completed MRI exams with adequate or excellent quality scores in TOF MRA. On average, the arterial diameters were larger for men than women, and vessels were more tortuous in men than women (Table 1). For each vessel segment, men tended to have larger arterial diameters and tortuosity at the A1 segment of ACA andM1 segment of MCA, after adjusting for age, race, intracranial volume, and presence of atherosclerosis. There were no significant differences in arterial diameters compared black to white participants, except for basilar arteries, which were larger in white participants (Table 2). Black participants had more tortuous arteries than white participants at the A1, M1, and basilar arteries, after adjusting for age, sex, intracranial volume, and the presence of atherosclerosis. Scan and reader reliability (Pearson correlation) ranged from 0.89 to 0.97 for the lumen diameter measurements. For vessel tortuosity, scan and reader reliability ranged from 0.58 to 0.96 (Table 3). Reliability estimates were consistently higher for basilar and vertebral arteries, compared to other vessel segments, with Bland-Altman plots showing good agreement without bias (p>0.05).Discussion
We have reported the quantitative measures of vessel tortuosity of the large intracranial arteries in a population-based study, which to date has been limited to qualitative assessments (i.e., lateral displacement of the basilar artery in relation to the clivus2,5). Quantifying the arterial diameters and degree of tortuosity will allow a longitudinal assessment of their change, providing a unique opportunity to prospectively study the role of NABAR and cognitive outcomes in ARIC neurocognitive studies.Conclusion
MRI measures of NABAR (quantified as luminal diameter and tortuosity) were reliable assessments in a US community-based population of older adults and showed differences by sex and race.Acknowledgements
This study is supported by NIH R21AG072244-01.References
1. Gutierrez,Jose, Cheung,Ken, Bagci,Ahmet, Rundek,Tatjana, Alperin,Noam, Sacco,Ralph, Elkind,Mitchell, Wright,Clinton. Brain Arterial Diameters as Biomarkers of Cognitive Performance: Results from the Northern Manhattan Study (P2.246). Neurology. 2016; 16: Supplement.
2. Gutierrez J, Kulick E, Park Moon Y, Dong C, Cheung K, Ahmet B, Stern Y, Alperin N, Rundek T, Sacco RL, Wright CB, Elkind MSV. Brain Arterial Diameters and Cognitive Performance: The Northern Manhattan Study. J Int Neuropsychol Soc. 2017; 1-12.
3. Shirwany NA, Zou MH. Arterial stiffness: a brief review. Acta Pharmacol Sin. 2010; 31: 1267-1276.
4. Duca L, Blaise S, Romier B, Laffargue M, Gayral S, El Btaouri H, Kawecki C, Guillot A, Martiny L, Debelle L, Maurice P. Matrix ageing and vascular impacts: focus on elastin fragmentation. Cardiovasc Res. 2016; 110: 298-308.
5. Zhai FF, Yan S, Li ML, Han F, Wang Q, Zhou LX, Ni J, Yao M, Zhang SY, Cui LY, Jin ZY, Zhu YC. Intracranial Arterial Dolichoectasia and Stenosis: Risk Factors and Relation to Cerebral Small Vessel Disease. Stroke. 2018; 49: 1135-1140.
Figures

Figure 1: TOF MRA depicting tortuous remodeling of the basilar artery in an ARIC participant (79 y/o white male). The lumen contours are automatically detected using 3D non-uniform rational b-splines (NURBS) modeling (A) (LAVA software, Leiden University, the Netherlands). The contoured basilar lumen/wall is unfolded in 2D long-axis view (B). Tortuosity is calculated based on the formula (C, D): Tortuosity = Arc/Chord. The arc is the length of the centerline of the vessel segment, and chord is the straight distance between proximal and distal points.
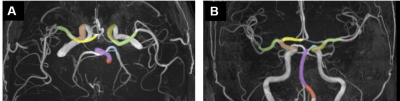
Figure 2: Quantitative measurements were obtained for standard vessel segments as shown on axial (A) and coronal views (B) of TOF MRA. Supraclinoid ICA, brown; M1 of MCA, green; dominant A1 of ACA (yellow); dominant P1 of PCA (blue), BA (magenta); V4 of VA (orange).