1771
GABA and Glutamate/Glutamine concentrations in the dACC of amphetamine treated adult ADHD patients
Yasmin Geiger1, Marganit Gonen-Shahar2, Gabriel Vainstein3, Angela Ruban2, and Assaf Tal1
1Weizmann Institute of Science, Rehovot, Israel, 2Tel Aviv University, Tel Aviv, Israel, 3Maccabi Healthcare, Kefar Sava, Israel
1Weizmann Institute of Science, Rehovot, Israel, 2Tel Aviv University, Tel Aviv, Israel, 3Maccabi Healthcare, Kefar Sava, Israel
Synopsis
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by irregular levels of hyperactivity, impulsivity and inattention. It is commonly linked to dopamine and norepinephrine balance. Several studies suggested connections to γ-amino butyric acid (GABA) and glutamate (Glu) imbalance in the dorsal anterior cingulate cortex (dACC). Here we use 1H-MRS to study GABA and glutamate + glutamine (Glx) levels in the dACC of ADHD patients, before and after pharmacological treatment and compared to healthy adults. We found no metabolic difference between ADHD and control group and no change after amphetamine treatment. We found no metabolic correlation to ADHD scores.
Introduction
Attention deficit hyperactivity disorder (ADHD) is a common neurodevelopmental disorders with prevalence rates of 7.2 %[1]. The cingulo-frontal-parietal (CFP) network is responsible for executive functioning and displays functional abnormalities in ADHD patients [2]. ADHD is commonly linked to dopamine and norepinephrine deficiency [3]. ADHD symptoms can be reduced using methylphenidate (such as Ritalin) or amphetamine (as Adderall) based medication which target dopamine transporters. Recent studies show GABA and Glutamate are disturbed across the CFP network in subjects with ADHD [4-7]. However, these results are inconsistent. Showing changes in one metabolic system but not the other or no changes to GABA or Glx. The dorsal anterior cingulate cortex (dACC), part of the CFP network, is responsible for decision making and allocation of cognitive control [8]. Here we examine metabolic changes, induced by Adderall, at the dACC of ADHD patient compared to healthy adults using 1H-MRS in 3T MRI scanner.Methods
Cohort: 12 adults (5F, age 25.1 ± 3.1, mean ± standard deviation) diagnosed with ADHD by neurologist and treated medically with amphetamines (Adderall) and 10 healthy adults (6F, age 25.6 ± 3.4, mean ± standard deviation) enrolled from the Maccabi Health Services database and gave informed consent. ADHD patients withheld stimulant medication three days prior to the MRS scan. Scores of inattention (IA) and hyper-activity (HA) were assessed for all volunteers, based on self-reported questionnaires (ASRS and DSM). Exclusion criteria included current use of neurological or psychiatric medication. Control volunteers with IA or HA scores > 16 (ASRS) or > 5 (DSM) were excluded.MRI and MRS: Scans were carried out on Siemens 3-T Prisma (Siemens-Healthineers, Erlangen, Germany) using 32-channel coil. Structural images were acquired using sagittal magnetization prepared rapid gradient echo (MPRAGE) sequence. 1H‑MRS spectra were acquired from 10 mL voxel at the dACC. Spectra were acquired using MEGAPRESS [9, 10], with TR/TE = 3000/68 ms and 14 ms sinc-Gaussian editing pulses applied interleaved at 7.5 ppm and 1.9 ppm and 192 scans (TA=9:48 min). ADHD patients were initially scanned after three days without pharmacological treatment, and then removed from the magnet, administered 10 ms of Adderall, and rescanned after 90 minutes. The scanning protocol was identical for both scans.
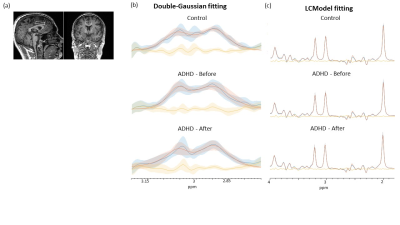
Post-processing: 1H-MRS Spectra, fitting and voxel placement are in figure 2. GABA+ concentrations calculated using double-Gaussian fitting to the 3.0 ppm resonance in the MEGAPRESS difference spectra, using in-house routines written (VDI software, The Weizmann Institute, Israel; www.vdisoftware.net ) in MATLAB 2020a (The Mathworks, Natick MA). Additional metabolic concentrations were derived from the un-edited MEGAPRESS, using LCModel v6.3 [13] with a simulated basis set containing 16 metabolites. Concentrations with CRLB<15% were discarded. Metabolic concentrations were corrected for partial volume effect [122, 123].
Results
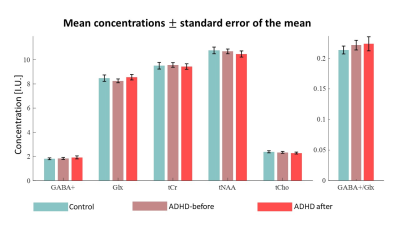
GABA, Glx (Glu+Gln), Cr, NAA, Cho and mI concentrations were analyzed and correlated to IA and HA scores. In the ADHD group we found no change in the concentration of any metabolite after administration/consumption of Adderall (10 mg) using t-test analysis. No significant difference in concentrations were observed between ADHD and control group. No linear correlations were observed between metabolic concentrations and ASRS or DSM scores for inattention and hyper-activity.Discussion and Conclusion
We found no changes to GABA, Glx or their ratio in the dACC of ADHD patients compared with healthy volunteers. Intra-subject analysis did not show any effect of amphetamine on metabolites concentrations. Our preliminary results are similar to the results of a large meta-analysis and clinical studies that did not find any difference in neurotransmitters concentration in the dACC between ADHD patients and control [11-14].Acknowledgements
Assaf Tal acknowledges the support of the Israeli Science Foundation (personal grant 416/20), the Monroy‐Marks Career Development Fund, and the historic generosity of the Harold Perlman FamilyReferences
- Thomas, R., et al., Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics, 2015. 135(4): p. e994-e1001.
- Bauer, J., et al., Hyperactivity and impulsivity in adult attention-deficit/hyperactivity disorder is related to glutamatergic dysfunction in the anterior cingulate cortex. The World Journal of Biological Psychiatry, 2018. 19(7): p. 538-546.
- Mamiya, P.C., A.B. Arnett, and M.A. Stein, Precision medicine care in ADHD: The case for neural excitation and inhibition. Brain Sciences, 2021. 11(1): p. 91.
- Maltezos, S., et al., Glutamate/glutamine and neuronal integrity in adults with ADHD: a proton MRS study. Translational psychiatry, 2014. 4(3): p. e373-e373.
- Naaijen, J., et al., Fronto-striatal glutamatergic compounds in compulsive and impulsive syndromes: a review of magnetic resonance spectroscopy studies. Neuroscience & Biobehavioral Reviews, 2015. 52: p. 74-88.
- Edden, R.A., et al., Reduced GABA concentration in attention-deficit/hyperactivity disorder. Archives of general psychiatry, 2012. 69(7): p. 750-753.
- Mamiya, P.C., et al., Task-related excitatory/inhibitory ratios in the fronto-striatal circuitry predict attention control deficits in attention-deficit/hyperactivity disorder. medRxiv, 2021.
- Shenhav, A., J.D. Cohen, and M.M. Botvinick, Dorsal anterior cingulate cortex and the value of control. Nature neuroscience, 2016. 19(10): p. 1286-1291.
- Tremblay, S., et al., The Use of Magnetic Resonance Spectroscopy as a Tool for the Measurement of Bi-hemispheric Transcranial Electric Stimulation Effects on Primary Motor Cortex Metabolism. Jove-Journal of Visualized Experiments, 2014(93).
- Marjanska, M., et al., Brain dynamic neurochemical changes in dystonic patients: a magnetic resonance spectroscopy study. Mov Disord, 2013. 28(2): p. 201-9.
- Maier, S., et al., Effects of 12-Week Methylphenidate Treatment on Neurometabolism in Adult Patients with ADHD: The First Double-Blind Placebo-Controlled MR Spectroscopy Study. Journal of Clinical Medicine, 2020. 9(8): p. 2601.
- Endres, D., et al., Normal neurochemistry in the prefrontal and cerebellar brain of adults with attention-deficit hyperactivity disorder. Frontiers in behavioral neuroscience, 2015. 9: p. 242.
- Schür, R.R., et al., Brain GABA levels across psychiatric disorders: A systematic literature review and meta‐analysis of 1H‐MRS studies. Human brain mapping, 2016. 37(9): p. 3337-3352.
- Perlov, E., et al., Spectroscopic findings in attention-deficit/hyperactivity disorder: review and meta-analysis. The World Journal of Biological Psychiatry, 2009. 10(4-2): p. 355-365.
Figures
Figure
1. (a) Voxel placement. Averaged and SD of measured spectra
(blue),fitting (red) and the residual from their subtracting (yellow) for the (b) Difference
spectra and (c) un-edited spectra.
Figure
2. Mean metabolic concentrations in ADHD patients before and after
administration of 10 mg Adderall, and in control group. Error bars represent
the standard error of the mean.
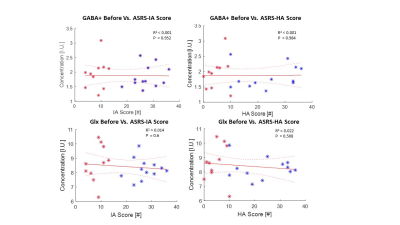
Figure 3. Correlations between basal GABA and Glx concentrations and IA and
HA scores from the ASRS test. No correlation was observed for either
neurotransmitter.
DOI: https://doi.org/10.58530/2022/1771