1752
Diagnosis and Follow-up of cervical vascular dissection using 3D MR vessel wall imaging: A Single Centre Experience of 65 Cases1Radiology, Renji Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, China, 2Renji Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, China, 3Philips Healthcare, Shanghai, China, 4Biomedical Engineering & Center for Biomedical Imaging Research, Tsinghua University, Beijing, China, 5University of Washington, Seattle, WA, United States
Synopsis
Cervical artery dissection (CAD) is one of the important causes of ischemic stroke in young and middle-aged people[1; 2]. DSA remains the gold standard for identifying and characterizing carotid vascular dissections[3]. However, this imaging approach is known to have certain limitations, including invasiveness, ionizing radiation exposure, uneconomic, and inconvenience in follow-up. Recently, rapid three-dimensional MR vessel wall imaging (3D MR-VWI) techniques have been developed to visualize arterial lumen and outer wall boundaries non-invasively and without contrast administration. Non-invasive 3D MR-VWI has the potential to be a powerful tool for follow-up of cervical artery dissection.
Introduction
Cervical artery dissection (CAD) is one of the important causes of ischemic stroke in young and middle-aged people[1; 2]. DSA remains the gold standard for identifying and characterizing carotid vascular dissections[3]. However, this imaging approach is known to have certain limitations, including invasiveness, ionizing radiation exposure, uneconomic, and inconvenience in follow-up. Recently, rapid three-dimensional MR vessel wall imaging (3D MR-VWI) techniques have been developed to visualize arterial lumen and outer wall boundaries non-invasively and without contrast administration[4; 5]. This study investigated the imaging features of CAD on 3D MR-VWI and analyzed the influential factors of vascular recanalization.Methods
Study population: Patients who were made a definite diagnosis of CAD were recruited in our study. During the hospitalization, patients all underwent the 3D MR-VWI examination for detailed assessment. The enrolled patients were recommended for the 3D MR-VWI reexamination as a follow-up after the conservative or surgical treatment. MR Imaging: 3D MR-VWI was performed on a 3T whole-body MR scanner (Ingenia, Philips Healthcare Systems, the Netherlands) with a 16-channel head coil and an 8-channel dedicated surface neck coil. The carotid arteries were imaged with 3D T1-VISTA with the following paraments: TR/TE 800/19ms, flip angle 90°, field of view (FOV) 200×180×40mm3, voxel size 0.5×0.5×0.5mm3.Results
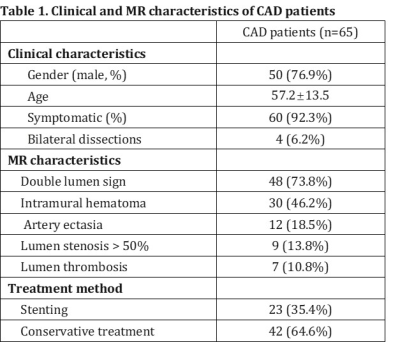
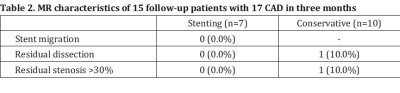
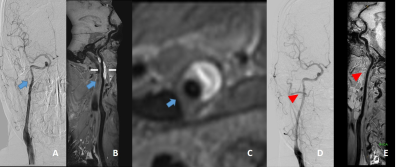
In this study, 65 patients diagnosed with CAD by both 3D MR-VWI and DSA were recruited. Clinical and MR characteristics of CAD patients were recorded in table 1. 23.1% (15/65) of the enrolled patients underwent the 3D MR-VWI reexamination in our hospital at least one time after conservative or surgical treatment. Among them, 13 patients had unilateral, and 2 had bilateral dissections in the past medical history in our hospital. 7 targeted arteries were stented, while 10 underwent conservative treatment. During follow-up, all the arteries can be effectively assessed on the 3D MR-VWI images. No residual dissection or stenosis>30% was found in the stented arteries in the 3 months’ follow-up. In the conservative treatment group, 10% arteries remained residual dissection and stenosis>30% in the 3 months’ follow-up. The detailed information was recorded in table 2.Discussion
3D MR-VWI techniques have abilities to visualize both arterial lumen and outer wall boundaries. The tearing and outlet of intima, false lumen of the vessel wall, and intramural hematoma could all be detected by 3D MR-VWI. In the follow-up, 3D MR-VWI can well display whether the stent is in place or the intramural hematoma is absorbed.Conclusion
Non-invasive 3D MR-VWI has the potential to be a powerful tool for follow-up of cervical artery dissection.Acknowledgements
NoneReferences
1 Yuan X, Cui X, Gu H et al (2020) Evaluating cervical artery dissections in young adults: a comparison study between high-resolution MRI and CT angiography. Int J Cardiovasc Imaging. 10.1007/s10554-020-01799-4
2 Hakimi R, Sivakumar S (2019) Imaging of Carotid Dissection. Curr Pain Headache Rep 23:2
3 Wang Y, Lou X, Li Y et al (2014) Imaging investigation of intracranial arterial dissecting aneurysms by using 3 T high-resolution MRI and DSA: from the interventional neuroradiologists' view. Acta Neurochir (Wien) 156:515-525
4 Zhao H, Wang J, Liu X et al (2015) Assessment of Carotid Artery Atherosclerotic Disease by Using Three-dimensional Fast Black-Blood MR Imaging: Comparison with DSA. Radiology 274:508-516
5 Han M, Rim NJ, Lee JS, Kim SY, Choi JW (2014) Feasibility of high-resolution MR imaging for the diagnosis of intracranial vertebrobasilar artery dissection. Eur Radiol 24:3017-3024
Figures