1663
Evaluation of diastolic (dys-)function using CMR feature tracking in all four cardiac chambers1Department of Radiology, University Hospital of Cologne, Cologne, Germany, 2Department of Radiology, University Hospital of Würzburg, Würzburg, Germany
Synopsis
Due to demographic changes, the prevalence of cardiac conditions predisposing to diastolic dysfunction (DD) is rising steadily. The main focus of non-invasive assessment of parameters for DD has been on left ventricular strain alterations. In this prospective study, we performed strain analysis of all 4 cardiac chambers using cardiac magnetic resonance feature tracking in patients with echocardiographically diagnosed DD and compared the results to a healthy control group. Left atrial strain parameters proved to be the most potent predictors of DD and allowed for a clear separation between patients and age-matched controls.
Introduction
With the rising prevalence of conditions predisposing to heart failure with preserved ejection fraction (HFpEF), non-invasive assessment of diastolic (dys-)function (DD) is becoming increasingly important1,2. The current diagnostic gold standard – the invasive measurement of left ventricular (LV) filling pressures, is not feasible for clinical routine use and follow-up3,4. Non-invasive parameters, such as echocardiographic measurement of mitral inflow and LV strain proved to be a good surrogate of LV filling pressure5-8. Nevertheless, the need for high image quality and examiner dependent expertise represents a limitation of this imaging modality. Cardiac magnetic resonance (CMR) is a highly reproducible and robust imaging alternative9,10.In the past, most studies focused on LV strain parameters for the detection of DD. However, since the 4 chambers of the heart are both anatomically and functionally interconnected, it appears reasonable to assume that strain analysis of the other heart cavities could also provide valuable information. In the present prospective study, we aimed to assess the diagnostic value of individual LV, right ventricular (RV), left atrial (LA), and right atrial (RA) strain parameters in patients with HFpEF using CMR feature tracking (FT).
Methods
A total of 27 patients with echocardiographically diagnosed DD and preserved LV EF underwent CMR (Ingenia 3T, Philips, Best, The Netherlands ). Clinical diagnosis of HFpEF was based on the current guidelines of the European Society of Cardiology. Exclusion criteria were: 1) cardiac arrhythmias, 2) history of myocardial infarction, 3) New York Heart Association class IV heart failure, and 4) general contraindications for CMR. Additionally, 18 healthy subjects were examined and served as controls.The CMR protocol included cine images in three long axis (2-, 3- and 4-chamber) views and a short-axis stack. Standard functional analysis was performed using a dedicated postprocessing platform (ISP Version 8, Philips). Analyses of global longitudinal strain and strain rate (SR) of all 4 chambers as well as global circumferential and radial strain with corresponding SR of both ventricles were performed using a dedicated FT-software (Medviso Segment, Version v2.1 R5891). As previously described11, atrial performance was evaluated regarding reservoir (total strain [Es], peak positive SR [SRs]), conduit (passive strain [Ee], early peak negative SR [SRe]) and booster pump function (active strain [Ea], late peak negative SR [SRa]).
Statistical analysis was performed using Welch’s independent T-test and logistic regression.
Results
No significant differences were found between HFpEF-patients and controls with respect to demographic data, except for age (78.8 ± 9.1 vs 62.7 ± 5.7 years, p<0.001) and gender (p=0.043). In volumetric analysis, a significantly increased wall mass of HFpEF patients could be observed (58.95 ± 20.9 vs. 34.99 ± 6.66 g/m2, p=0.002). LV and RV EF were not significantly different between the HFpEF-group and controls (74.67 ± 9.26 vs. 71.86 ± 4.63 and 54.67 ± 9.3 vs. 51.71 ± 9.23, p>0.05 respectively).Regarding ventricular strain parameters, only LV global radial SRs of HFpEF-patients was significantly impaired when compared to controls (p=0.034). In contrast, LA strain parameters referring to different phases of atrial function allowed for a clear separation between both groups (Figure 1). Particularly SR parameters reflecting LA reservoir (SRs: p<0.001, Es: p=0,003) and conduit function (SRe: p=0.001) showed highly significant differences (Table 1). The best discriminatory potential could be demonstrated for LA SRe and Es (area under the curve=0.85; sensitivity=77 %, specificity=87 %; Figure 2). The addition of LV or RV parameters to the model did not lead to an improvement of predictive potential.
Discussion
To our knowledge this is the first CMR study to evaluate strain and SR parameters of all 4 cardiac chambers. The results of the present study indicate, that LA parameters are the most potent strain predictors for the presence of HFpEF.Particularly reservoir function parameters showed to be significantly reduced. Impaired dilatation of the LA indicates a reduced atrial compliance and filling, thus affecting LV diastolic function. Similarly, conduit and booster function are affected by LV compliance and pressure, showing a reduced LA contractility. Interestingly, in the context of LA reservoir and conduit function, particularly SR – meaning the velocity of myocardial deformation – was reduced. This could indicate a higher time-sensitivity of atrial dysfunction.
In echocardiography, stages of DD are primarily based on the assessment of early and late mitral inflow (E- and A-wave), reflecting passive and active LV filling, respectively12. Early mitral inflow physiologically corresponds to atrial conduit function, and late mitral inflow to atrial booster function. Following this reasoning, it may be concluded that physiologically corresponding CMR strain parameters of the LA show similar changes and could as well be used for diagnosis of DD.
A relevant limitation to this work is the lack of invasive LV pressure measurements. Nevertheless, CMR has the potential to deliver better reproducible functional data compared to echocardiography, and additional information on tissue properties, allowing for a more comprehensive diagnosis1,3,6. To that end, future studies examining various degrees of DD are necessary.
Conclusion
LA strain parameters might be more sensitive in the detection of altered myocardial function when compared to LV strain. Especially LA SRe and Es represent useful non-invasive surrogate parameters for LV diastolic function and allow for a clear separation between HFpEF-patients and the control group.Acknowledgements
Special thanks to Hannah Disse, Melanie Treutlein and Fabian Kuhl.References
1. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129-2200.
2. Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32(6):670-679.
3. Webb J, Fovargue L, Tondel K, et al. The Emerging Role of Cardiac Magnetic Resonance Imaging in the Evaluation of Patients with HFpEF. Curr Heart Fail Rep. 2018;15(1):1-9.
4. Khouri SJ, Maly GT, Suh DD, et al. A practical approach to the echocardiographic evaluation of diastolic function. J Am Soc Echocardiogr. 2004;17(3):290-297.
5. Appleton CP, Galloway JM, Gonzalez MS, et al. Estimation of left ventricular filling pressures using two-dimensional and Doppler echocardiography in adult patients with cardiac disease. Additional value of analyzing left atrial size, left atrial ejection fraction and the difference in duration of pulmonary venous and mitral flow velocity at atrial contraction. J Am Coll Cardiol. 1993;22(7):1972-1982.
6. Daneshvar D, Wei J, Tolstrup K, et al. Diastolic dysfunction: improved understanding using emerging imaging techniques. Am Heart J. 2010;160(3):394-404.
7. Nagueh SF. Non-invasive assessment of left ventricular filling pressure. Eur J Heart Fail. 2018;20(1):38-48.
8. Mandoli GE, Sisti N, Mondillo S, et al. Left atrial strain in left ventricular diastolic dysfunction: have we finally found the missing piece of the puzzle? Heart Fail Rev. 2020;25(3):409-417.
9. Grothues F, Smith GC, Moon JC, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol. 2002;90(1):29-34.
10. Chamsi-Pasha MA, Zhan Y, Debs D, et al. CMR in the Evaluation of Diastolic Dysfunction and Phenotyping of HFpEF: Current Role and Future Perspectives. JACC Cardiovasc Imaging. 2020;13(1 Pt 2):283-296.
11. Kowallick JT, Kutty S, Edelmann F, et al. Quantification of left atrial strain and strain rate using cardiovascular magnetic resonance myocardial feature tracking. Journal of Cardiovascular Magnetic Resonance. 2015;17(Suppl 1):P66.
12. Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17(12):1321-1360.
Figures

Table 1: LA strain parameters
LA = left atrium, E = strain, SR = strain rate, Es = total strain, Ee = passive strain, Ea = active strain, SRs = peak positive SR, SRe = early peak negative SR, SRa = late peak negative SR, HFpEF = heart failure with preserved ejection fraction.
Data are given as mean ± standard deviation. p values in bold are statistically significant.
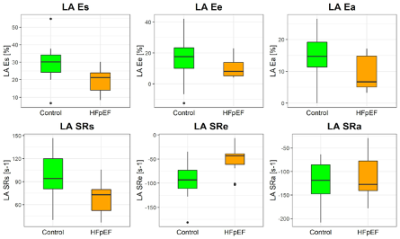
Figure 1: LA strain parameters
Box-Whisker plots illustrating differences in LA strain parameters between HFpEF-patients and control group. * = p<0.05, ** = p< 0.01, *** = p< 0.001
LA = left atrium, E = strain, SR = strain rate, Es = total strain, Ee = passive strain, Ea = active strain, SRs = peak positive SR, SRe = early peak negative SR, SRa = late peak negative SR, HFpEF = heart failure with preserved ejection fraction.
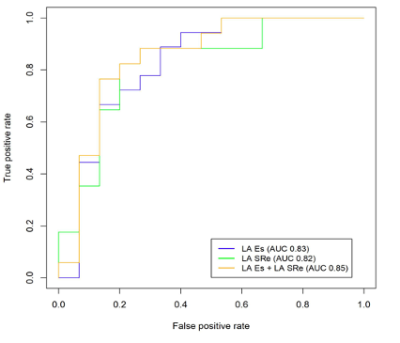
Figure 2: Receiver operating characteristic (ROC) analyses for prediction of diastolic dysfunction
LA = left atrium, Es = total strain, SRe = early peak negative strain rate, AUC = area under the curve.