1595
Assessment of the Diagnosis Value of Diffusion Tensor Imaging and Fractional Anisotropy Value in Peripheral Prostate Cancer based on PI-RADS v21Radiology, The Department of Radiology, General Hospital of Ningxia Medical University, Yinchuan, China, 2GE Healthcare, MR Research China, Beijing, Beijing, China
Synopsis
In this retrospective study, we aim to explore the diagnostic values of diffusion tensor imaging (DTI) in peripheral prostate cancer, and compare DTI with diffusion weighted imaging (DWI) based on prostate imaging reporting and data system version 2 (PI-RADS v2) in peripheral prostate cancer (PCa). It was concluded that both DWI and DTI have high values in the diagnosis and differentiation of PCa, and DWI& dynamic contrast enhanced (DCE) MRI has higher diagnostic efficiency than DTI&DCE-MRI according to PI-RADS v2.
Introduction
Diffusion tensor imaging (DTI) technique can derive multiple quantitative indexes, such as apparent diffusion coefficient (ADC) and fractional anisotropy (FA), which can quantitatively reflect physiological features and pathological changes at microscopic level[1]. The measurement of ADC value is helpful to the differential diagnosis and quantitative evaluation of prognosis of prostate cancer (PCa)[2]. However, the reported studies are still controversial on the application of FA value, and most scholars believe that it may be related to multiple factors such as sample differences, imaging equipment, and pathological characteristics of cancer foci. The recommended scan protocol in prostate imaging reporting and data system version 2.0 (PI-RADS v2) includes three sequences: T2-weighted imaging (T2WI), diffusion weighted imaging (DWI) and dynamic contrast enhanced (DCE) MRI, while the peripheral zone lesions were mainly scored by DWI and ADC value[3,4]. In this study, we compared the diagnostic value of DTI&FA value and DWI&ADC value in peripheral PCa, using a 5-point scale according to the DWI scoring standard in PI-RADS v2.Material and Methods
Our Institutional Review Board has approved this study and written informed consent was obtained from each patient. Retrospectively, 30 patients prostatic peripheral zone cancer patients (malignant group), with an average age of (68.5 ± 8.9) years and 48 benign prostate hyperplasia (BPH) and/or chronic prostatitis (CP) patients (benignant group) with an average age of (67.6 ± 9.2) years were enrolled by image analysis and biopsy proven. All MR examinations were performed with a 3.0T MR scanner (Signa Excite HD 3.0, GE Healthcare, Milwaukee, WI) equipped with a 32-channel phased-array coil. For each patient, an image dataset including T2WI, DWI, DTI and DCE-MRI was collected. The main scan parameters were listed in Table 1.The DTI images and FA values were scored by using the criteria of DWI in PI-RADS v2. Receiver operating characteristic (ROC) curves were used to compare the diagnostic efficiency among T2WI, DWI, DTI, DCE-MRI, DWI&DCE-MRI and DTI&DCE-MRI based on PI-RADS v2.
Results
Table 2 shows the group composition and the corresponding Gleason scores. The receiver operating characteristic (ROC) curves were drawn (shown in Figure 1) and the area under the curve (AUC) was then calculated subsequently. The AUC and the 95% confidence interval (CI) of different technique schemes were listed in Table 2, while the diagnostic effectiveness was shown in Table 3. Based on PI-RADS v2, DWI&DCE-MRI had the highest sensitivity (90.0%), followed by DTI&DCE-MRI (83.3%), while DTI alone had the highest specificity (89.6%), and DWI or DTI alone had the highest accuracy (84.6%).Discussion and Conclusion
Based on PI-RADS v2, our results have demonstrated that both the DWI and DTI have high values in the diagnosis and differentiation of PCa, while the DWI&DCE-MRI has higher diagnostic efficiency than DTI&DCE-MRI. The sensitivity, specificity and AUC values of DTI in the diagnosis of PCa are consistent with the results of previous study[5].Many scholars are still arguing about the effectiveness of DTI in the diagnosis of PCa. Gibbs et al[6] claimed that ADC was more effective than FA value in the diagnosis of PCa, while the combination of ADC and FA values did not perform better. Yoon et al[7] showed that FA value had higher effectiveness in the diagnosis of PCa than ADC value. Our study showed that DWI alone had higher diagnostic effectiveness in peripheral PCa than DTI (0.867>0.845, P<0.05), which is more similar to the results of Gibbs et al[6].
In our study, the DTI images were evaluated by reference to the scoring criteria of DWI in PI-RADS v2, and the results showed that the AUC of DWI&DCE-MRI was higher than the AUC of DTI&DCE-MRI for PCa diagnosis. (0.884>0.851, P<0.05). One of the major limitations in our study is that the pathological results as the “gold standard” in this study mainly come from puncture biopsy, which is easy to miss small cancer foci, and is an objective systemic error that cannot be completely avoided.
In conclusion, both DWI and DTI have high values in the diagnosis and differentiation of PCa, and the DWI&DCE-MRI scheme has higher diagnostic efficiency than the DTI&DCE-MRI scheme according to PI-RADS v2.
Acknowledgements
The authors thank Mrss Tao Wang, Mrss Ting Huang, and Mr Zichao Zhu for helping in gathering and analyzing the data.
References
[1]. Bammer R, Acar B, Moseley M E. In vivo MR tractography using diffusion imaging[J]. European journal of radiology, 2003, 45(3): 223-234.
[2]. Manetta R, Palumbo P, Gianneramo C, et al. Correlation between ADC values and Gleason score in evaluation of prostate cancer: multicentre experience and review of the literature[J]. Gland surgery, 2019, 8: S216.
[3]. Padhani A R, Weinreb J, Rosenkrantz A B, et al. Prostate imaging-reporting and data system steering committee: PI-RADS v2 status update and future directions[J]. European urology, 2019, 75(3): 385-396.
[4]. Weinreb J C, Barentsz J O, Choyke P L, et al. PI-RADS prostate imaging–reporting and data system: 2015, version 2[J]. European urology, 2016, 69(1): 16-40.
[5]. Katahira K, Takahara T, Kwee T C, et al. Ultra-high-b-value diffusion-weighted MR imaging for the detection of prostate cancer: evaluation in 201 cases with histopathological correlation[J]. European radiology, 2011, 21(1): 188-196.
[6]. Gibbs P, Pickles M D, Turnbull L W. Diffusion imaging of the prostate at 3.0 tesla[J]. Investigative radiology, 2006, 41(2): 185-188.
[7]. Yoon S K, Kim D W, Ha D H, et al. Value of diffusion tensor imaging of prostate cancer: comparison with systemic prostate biopsy[J]. Journal of the Korean Society of Radiology, 2011, 64(2): 179-184.
Figures
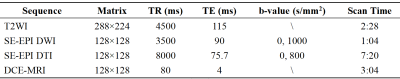
Table 1. The main scan parameters of this study
* Field of view (FOV): 360 × 360 mm2; slice thickness: 3 mm; slice gap: 0 mm; all images were collected in transverse view.
**For DTI, the diffusion gradients were applied in 25 directions.
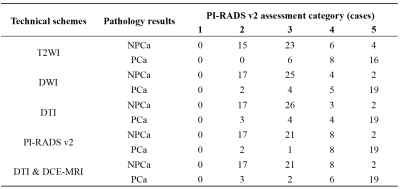
Table 2. Assessment category and pathology results of different MR sequences
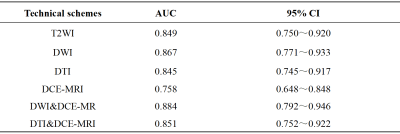
Table 3. The AUC and 95% CI of different imaging schemes in the diagnosis of PCa
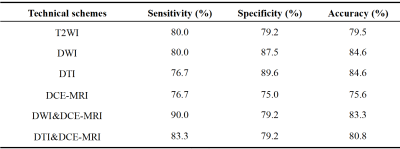
Table 4. Diagnostic effectiveness of different imaging schemes in the diagnosis of PCa
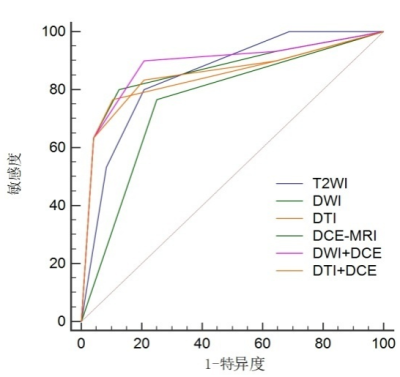
Figure 1. ROC curves characteristic the diagnostic effectiveness of T2WI, DWI, DTI, DCE-MRI and DWI&DCE-MRI, DTI&DCE-MRI in the diagnosis of PCa