1588
Mammography-like MR images using a preconditioned water-fat-silicone total field inversion QSM algorithm1Department of Diagnostic and Interventional Radiology, School of Medicine, Klinikum Rechts der Isar, Technical University of Munich, Munich, Germany, 2Philips Research, Hamburg, Germany, 3Philips GmbH Market DACH, Hamburg, Germany
Synopsis
Early stage malignant tumors are often accompanied by microcalcifications. X-ray-based mammography examinations are routinely used for screening and early detection due to the excellent contrast of calcified structures. However, due to the damaging nature of x-ray radiation, the use of an MR-based technique would be desirable for repeated examinations. In this work, we present initial results of quantitative-susceptibility-mapping-based (QSM) mammography-like MR-images that show robust detection of calcifications down to the resolution of the MR scan. Furthermore, the proposed method accounts for the potential presence of silicone breast implants allowing robust QSM in proximity to silicone implants for the first time.
Introduction
Breast calcifications are common and mostly benign, but certain distributions of especially microcalcifications constitute a marker of malignancy. Mammography is currently considered the “gold standard” for detection and characterization of breast calcifications. However, existing clinical breast MRI examinations cannot detect and characterize breast calcifications. Quantitative susceptibility mapping is a common methodology to assess calcifications with MRI1 and some early works have reported on the ability to detect breast calcifications with QSM2,3,4. However,QSM remains challenged by the presence of multiple species (water, fat and potentially silicone) in the breast. Water–fat total field inversion enables QSM in the presence of fat5 and a novel graph-cut algorithm has been proposed for water–fat–silicone separation6. The present work proposes a preconditioned water–fat–silicone total field inversion QSM algorithm to enable Mammography-like MRI of breast calcifications.Methods
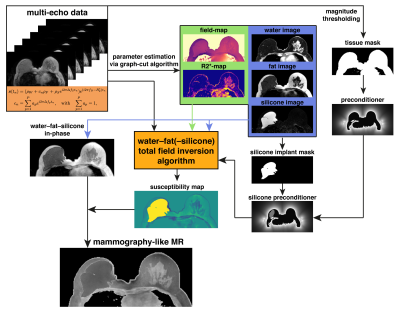
The proposed mammography-like magnetic resonance (MR) contrast algorithm consists of three main steps (Fig.1). First, the water-, fat- and silicone-image, field-map and $$$R_2^*$$$ were estimated using a hierarchical multi-resolution graph-cut algorithm based on6,7. Based on the silicone image, silicone implants were identified and a silicone-implant-mask was$$$\;$$$generated. Second, the susceptibility map was computed directly from complex multi-echo gradient-echo data by using a preconditioned water–fat–silicone total field inversion (wfsTFI) algorithm similar to5. The wfsTFI minimizes the following cost-function:$$y=\underset{y'}{\arg\min}=\sum_{j=1}^{N_{\text{echo}}} ||\left(\rho_W+c_n\rho_F+\rho_{s}e^{i2\pi\Delta{f_{S}}t_{j}}\right)e^{-R_2^*t_j}e^{i2\pi{t_j}\; d\:*Py'}-S_j||_2^2+\lambda{||}M_g\nabla{P}y'||_1\\c_n=\sum_{p=1}^{N_p}a_pe^{i2\pi\Delta{f_p}t_j},\quad\text{with}\quad\sum_{p=1}^{N_p}a_p=1,$$where $$$t_1,t_2,...,t_N$$$ are the different echo times, $$$d$$$ is the dipole kernel, $$$P$$$ is the preconditioner, $$$M_G$$$ is the MEDI-like edge mask8 and $$$\nabla$$$ is the gradient operation1, $$$\rho_W,\;\rho_F$$$, and $$$\rho_s$$$ are the complex signal of the water, fat, and silicone components assuming to have an equal transverse relaxation rate $$$R_2^*$$$. The final QSM map is computed as $$$\chi=Py$$$. The fat spectrum$$$\;$$$is assumed to have $$$N_p$$$ spectral peaks with corresponding relative amplitudes $$$a_p$$$ and chemical shift $$$\Delta{f_p}$$$. A multi-peak fat model specific to bone marrow9 was used. The preconditioner was automatically adapted to the ROI following10 for the background region and was set to 1 in the ROI. Furthermore, the silicone-implant-mask was included in the preconditioner, due to the strong susceptibility of silicone of around 2$$$\:$$$ppm.
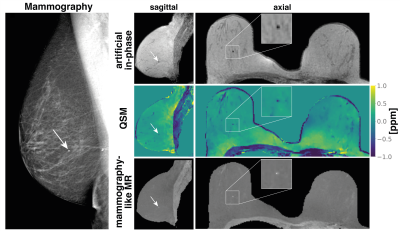
Mammography-like MR contrast
To generate a mammography-like contrast an artificial in-phase map was generated from the water, fat (, and silicone) separated images. The in-phase map was subsequently inverted to generate a inverted proton density contrast similar to x-ray attenuation-based mammography. Finally the inverted in-phase contrast was multiplied with the susceptibility map.
In vivo measurements
The above processing pipeline was applied to 3 patients with breast calcifications and available MR and mammography images. The mammography images served as a reference standard for the detection of calcifications. Scanning was performed on a 3$$$\:$$$T scanner (Ingenia, Philips Healthcare, Best, The Netherlands) using a monopolar time-interleaved multi-echo gradient echo sequence11, acquiring 6 echoes with 3 echoes per interleave. For all subjects the imaging parameters were set to TE$$$_{\text{min}}=1.58\:$$$ms,$$$\;\Delta$$$TE$$$=1.28\:$$$ms, FA$$$=3^{\circ}$$$,orientation$$$\;$$$=$$$\;$$$axial, readout direction$$$\;$$$=$$$\;$$$anterior-posterior, FOV$$$\:=220\times{382}\times{192}\:\text{mm}^3$$$, an isotropic acquisition voxel size of $$$1.3\:$$$mm$$$^3$$$, a compressed sensing factor of 6 and a total scan time of 4:15min.
Results
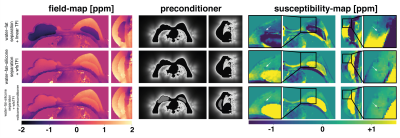
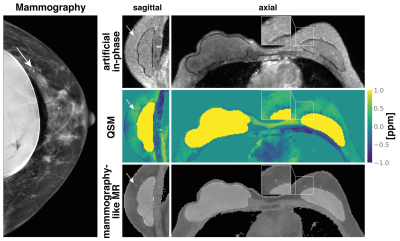
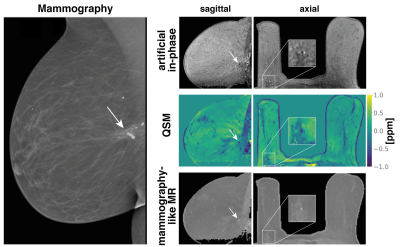
Modeling the chemical shift of silicone is necessary to estimate susceptibility close to silicone implants (Fig.2). Only the use of a preconditioner that includes the silicone implants allows for the assessment of susceptibility around the whole implant. In$$$\;$$$Fig.3 the same subject as in$$$\;$$$Fig.2 is shown including the attenuation-based mammography and the mammography-like MR image.The mammography-like image is in good agreement with the reference mammography and allows for the assessment of the calcification. This is also true in a second subject with a cluster of calcifications in dense tissue (Fig.4). The delineation between calcifications and fibrograndular tissue is hardly possible based only on the QSM map, since both tissues show hypointense values. The mammography-like image successfully suppresses the fibroglandular tissue and the calcification can easily be identified. Fig.5$$$\;$$$shows a third subject with the smallest calcification detected in the mammography-like images within the small cohort. The calcification is around$$$\;$$$1.5$$$\;$$$mm in diameter and thus slightly above the resolution of the MR scan.Discussion
The use$$$\;$$$of the proposed wfsTFI method for QSM followed by the generation of a mammography-like MR image allows for the reliable detection of calcifications slightly above the resolution of the MR scan. Due to the presently adapted preconditioner including regions of silicone,$$$\;$$$the detection is also possible for calcifications close to silicone implants in the proximity of the fibrous capsule. Furthermore, since the mammography-like MR image is 3D isotropic, it potentially overcomes limitations of conventional mammography where pathologies can be covered by other tissue or implants.However this preliminary study still has the limitation that microcalcifications, which are of high clinical relevance, were not detected due to the limited resolution. For a QSM-based detection of$$$\;$$$a calcification, the resolution of the MR scan needs to be above the size of the calcification. Partial volume effects limit the visualization of calcification of$$$\;$$$the size of$$$\;$$$only one voxel$$$\;$$$or below.
Furthermore, the employed sequence additionally allows for the assessment of breast density via proton density fat fraction and the assessment of implant integrity via the silicone separated image.
Conclusion
A novel preconditioned water-fat-silicone total field inversion QSM algorithm was proposed. The presented initial results show that a mammography-like contrast can be obtained using QSM for assessing calcifications down to the resolution of the QSM scan.Acknowledgements
The present work was supported by the European Research Council (grant agreement No 677661, ProFatMRI). The authors also acknowledge research support from Philips Healthcare.References
[1] Wang Y, Liu T. Quantitative Susceptibility Mapping (QSM): Decoding MRI Data for a Tissue Magnetic Biomarker. Magnetic Resonance in Medicine 2014; 73:82–101. 10.1002/mrm.25358.
[2] Dimov AV, Liu T, Spincemaille P, Ecanow JS, Tan H, Edelman RR,Wang Y. Joint Estimation of Chemical Shift and Quantitative Susceptibility Mapping (chemical QSM). Magnetic Resonance in Medicine 2014;73:2100–2110. 10.1002/mrm.25328.
[3] Schweser F, Hermann KH, Deistung A, Atterbury M, Baltzer PA, Burmeister HP, Kaiser WA, Reichenbach JR. Quantitative Magnetic Susceptibility Mapping (QSM) in Breast Disease Reveals Additional Information for MR-Based Characterization of Carcinoma Calcification. In: Proceedings 19.Annual Meeting International Society for Magnetic Resonance in Medicine,Montreal, 2011. p. 1014.
[4] Fatemi-Ardekani A, Boylan C, Noseworthy MD. Identification of breast calcification using magnetic resonance imaging. Medical Physics 2009;36:5429–5436. https://doi.org/10.1118/1.3250860.
[5] Boehm C, Sollmann N, Meineke J, Ruschke S, Dieckmeyer M, Weiss K, Zimmer C, Makowski MR, Baum T, Karampinos DC. Preconditioned water-fat total field inversion: Application to spine quantitative susceptibility mapping. ; n/a. https://doi.org/10.1002/mrm.28903.
[6] Stelter JK, Boehm C, Ruschke S, Diefenbach MN, Wu M, Weiss K, Borde T, Metz S, Makowski MR, Karampinos DC. Optimal experimental design for quantitative water, fat and silicone separation using a variable projection method with 4 or 6 echoes at 3T. Optimal experimental design for quantitative water, fat and silicone separation using a variable projection method with 4 or 6 echoes at 3T, 2021. p. 1517.
[7] Boehm C, Diefenbach MN, Makowski MR, Karampinos DC. ImprovedBody Quantitative Susceptibility Mapping By Using a Variable-layer Single-min-cut Graph-cut for Field-mapping. Magnetic Resonance inMedicine 2020; nil:mrm.28515. 10.1002/mrm.28515.
[8] Liu T, Liu J, de Rochefort L, Spincemaille P, Khalidov I, Ledoux JR,Wang Y. Morphology Enabled Dipole Inversion (MEDI) From a Single-Angle Acquisition: Comparison With Cosmos in Human Brain Imaging. Magnetic Resonance in Medicine 2011; 66:777–783. 10.1002/mrm.22816.
[9] Ren J, Dimitrov I, Sherry AD, Malloy CR. Composition of Adipose Tissue and Marrow Fat in Humans By 1h Nmr At 7 Tesla. Journal of Lipid Research 2008; 49:2055–2062. 10.1194/jlr.d800010-jlr200.
[10] Liu Z, Wen Y, Spincemaille P, Zhang S, Yao Y, Nguyen TD, Wang Y. Automated Adaptive Preconditioner for Quantitative Susceptibility Mapping.Magnetic Resonance in Medicine 2019; 83:271–285. 10.1002/mrm.27900.
[11] Ruschke S, Eggers H, Kooijman H, Diefenbach MN, Baum T, Haase A, Rummeny EJ, Hu HH, Karampinos DC. Correction of Phase Errors in Quantitative Water–Fat Imaging Using a Monopolar Time-Interleaved Multi-Echo Gradient Echo Sequence. Magnetic Resonance in Medicine2016; 78:984–996. 10.1002/mrm.26485.
Figures