1577
The left atrial function in hypertension patients with left ventricular diastolic dysfunction:A myocardial MR strain study1Radiology, The Second Affiliated Hospital of Nanchang University, Nanchang, China, 2MR Research, GE Healthcare, Beijing, China
Synopsis
Heart failure with preserved ejection fraction(HFpEF)was evaluated by echocardiography commonly. In this study, we try to use Cardiovascular Magnetic Resonance Tissue-Tracking (CMR-TT) to assess left atrial (LA) function in hypertension patients (HP) with left ventricular diastolic dysfunction (LVDD). The results demonstrated that LA myocardial function decreased in HP with LVDD. LA myocardial strain parameters could detect sensitively the myocardial deformation of LVDD in HP. Total strain(εs) parameter was an excellent parameter for diagnose HFpEF and evaluating the degree of LVDD.
Synopsis
Heart failure with preserved ejection fraction(HFpEF)was evaluated by echocardiography commonly. In this study, we try to use Cardiovascular Magnetic Resonance Tissue-Tracking (CMR-TT) to assess left atrial (LA) function in hypertension patients (HP) with left ventricular diastolic dysfunction (LVDD). The results demonstrated that LA myocardial function decreased in HP with LVDD. LA myocardial strain parameters could detect sensitively the myocardial deformation of LVDD in HP. Total strain(εs) parameter was an excellent parameter for diagnose HFpEF and evaluating the degree of LVDD.Introduction
Hypertension is a common chronic cardiovascular disease and a most cause for HFpEF, which accounts for 75%-85%1. LVDD can be divided into abnormal diastolic function (ADF) and HFpEF according to the degree of diastolic restriction2. HFpEF, which makes up 35–50% of all heart failure cases3, has attracted more and more attention, especially the changes of LA function. Previous researches indicated the impairment of LA function can reflect the restriction of filling in the left ventricle, which suggest the LVDD, changes in LA function play a key role in the occurrence and development of LVDD in HP 4-6. But few studies have investigated the possibility of MRI to diagnose HFpEF and detect the difference of LA function in different stage of LV diastolic dysfunction. The purpose of this study was to investigate the potential role of LA strain for diagnosing the HFpEF and evaluating the degree of LVDD by CMR-TT.Methods
This study was approved by the Ethics Committee of the Second Affiliated hospital of Nanchang University, and all participants agreed with the written informed consent. 54 HP and 30 healthy controls were enrolled in this study. According to the degree of LVDD4,54 HP were classified into two groups: HFpEF(n=24) and ADF(n=30). All MRI data were acquired using a 3-Tesla scanner (Discovery 750W,GE Healthcare, US). Two- and four-chamber MRI images were analyzed with cardiovascular magnetic resonance tissue-tracking (CMR-TT), a package of CVI (Circle Cardiovascular Imaging, v.5.12, Calgary, AB, Canada). The calculated LA function parameters include reservoir (total strain [εs], peak positive strain rate [SRs]), conduct (passive strain [εe], peak early negative strain rate [SRe]) and booster pump (active strain [εa], late peak negative strain rate [SRa]) (Figure 1 shows the definition of these parameters). The average septal-lateral E/e’ ratio was obtained from echocardiographic for reference. Kruskal-Wallis with post hoc Dunn’s test, Spearman analysis, receiver operating characteristic curve and intra-class correlation coefficient analysis were applied for statistical analyses. A P value of <0.05 was regarded as statistically significant.Results
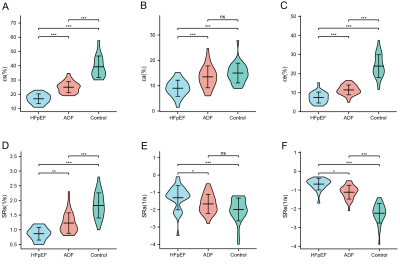
HFpEF patients had significantly lower absolute εs [17.1(14.65,19.275)], εa[8.85(7.425,11.325)], εe[7(5.075,9.55)], SRs [0.9(0.3,0.7)], SRa [-1.2(-1.4,-0.9)], SRe[-0.6(-0.825,-0.5)/s] than both ADF and control groups (P < 0.05 for all).Compared to control group, εs [1.1(0.1, 1) vs.1.8(1.45, 2.2)], εe [11.15(9.825, 13.575) vs.22.65(19.725, 29.15)] and SRs [1.1(1, 1.475) vs.1.8(1.45,2.2)] and SRe [-1, (-1.3, -0.9) vs.-2.2(-2.475, -1.9)] were all significantly impaired in ADF patients, except for εa and SRa (p<0.001for all)(Figure 2). The εs showed the highest diagnostic value for differentiating HFpEF patients from HTN patients (AUC, 0.954; cutoff value, 19.55/s; sensitivity, 96.7%; specificity, 79.2%). Also, the εs showed the highest diagnostic value for the differentiation of ADF patients and healthy (AUC, 0.983; cutoff value, 29.9/s; sensitivity, 90%; specificity, 100%)(Figure 4). Additionally, εs and εa was correlated with AS-L E/e' ratio respectively.(Figure 3)Discussion
Our study indicated that CMR-derived LA strain parameters demonstrated changes in LVDD, all LA functions impaired in HFpEF patients, but only reservoir and conduit function impaired in ADF patients, which indicate booster function have been preserved in early stage. This finding is in accord with previous literature7. Also,LA strain parameters were able to identify HFpEF and ADF patients. In previous study, left ventricular myocardial strain had been used to diagnose HFpEF8, but LA not. The LA strain, as a parameter based CMR-TT to evaluate the LA myocardial function,also showed excellent ability to diagnose HFpEF and evaluate the degree of left ventricular diastolic dysfunction. Moreover,εs and εa was weakly correlated with AS-L E/e' ratio, one parameter being used to reflect left ventricular diastolic function. Therefor,we believe εs is a good discriminator for diagnosing HFpEF and ADF in HP.Key Words
hypertension; heart failure with preserved ejection fraction; magnetic resonance imaging; left atrial myocardial strainAcknowledgements
We are grateful to Dr. Junhao Tu for valuable advice.References
1. Hicklin HE, Gilbert ON, Ye F, et al. Hypertension as a Road to Treatment of Heart Failure with Preserved Ejection Fraction. Current Hypertension Reports. 2020;22(10).
2. Pieske B, Tschöpe C, de Boer RA, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail. 2020 Mar;22(3):391-412.
3. Hicklin HE, Gilbert ON, Ye F, et al. Hypertension as a Road to Treatment of Heart Failure with Preserved Ejection Fraction. Current Hypertension Reports. 2020;22(10).
4. Khan MS, Memon MM, Murad MH, et al. Left atrial function in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Eur J Heart Fail. 2020;22(3):472-85.
5. Telles F, Nanayakkara S, Evans S, et al. Impaired left atrial strain predicts abnormal exercise haemodynamics in heart failure with preserved ejection fraction. Eur J Heart Fail. 2019;21(4):495-505.
6. Mandoli GE, Sisti N, Mondillo S, et al. Left atrial strain in left ventricular diastolic dysfunction: have we finally found the missing piece of the puzzle? Heart Fail Rev. 2020;25(3):409-17.
7. Li L, Chen X, Yin G, et al. Early detection of left atrial dysfunction assessed by CMR feature tracking in hypertensive patients. Eur Radiol. 2020 Feb;30(2):702-711.
8. He J, Sirajuddin A, Li S, et al. Heart Failure With Preserved Ejection Fraction in Hypertension Patients: A Myocardial MR Strain Study. J Magn Reson Imaging. 2021 Feb;53(2):527-539.
Figures
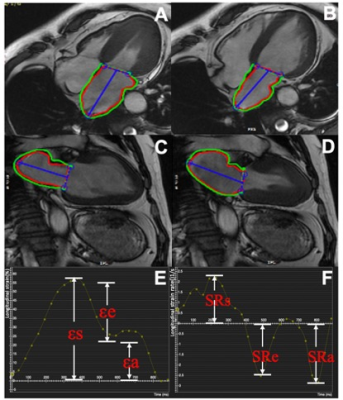
A case of left atrial strain and strain rate parameter from healthy control.
The endocardial and epicardial contours were manually drawn in the end-systolic and end-diastolic phases with the two-chamber, four-chamber views (A、B、C、D). The left atrial strain and strain rate curves (E、F)
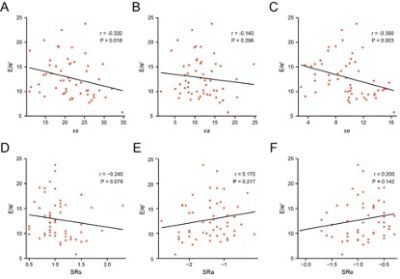
Correlations between left atrial strain parameters and average septal-lateral E/e' ratio.

ROC of left atrial parameters for differentiation of HFpEF patients with ADF patients(A)and ADF patients with healthy controls(B). HFpEF, Heart failure with preserved ejection fraction; ADF, Abnormal Diastolic Function.