1571
3D Whole Heart Grey-blood PSIR Imaging After Slow Infusion and Bolus Injection for High-resolution Isotropic LGE Imaging1School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom, 2Wellcome Centre for Human Neuroimaging, UCL Queen Square Institute of Neurology, University College London, London, United Kingdom, 3MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom
Synopsis
3D whole-heart free breathing water/fat non-rigid motion corrected grey-blood PSIR LGE technique has been recently proposed showing good agreement with conventional 2D grey-blood LGE MRI. Due to the relatively long scan time of ~10 minutes, contrast washout may influence scar detection and limit spatial resolution. Here we compare the proposed 3D grey-blood PSIR LGE after slow infusion and bolus injection at high isotropic spatial resolution to evaluate the benefit of the slow infusion injection. Both pipelines were compared to the conventional breath-held 2D grey blood PSIR-LGE imaging technique. Overall higher quality scores were observed in images acquired after slow infusion.
Introduction
Recently proposed 3D whole heart free-breathing motion corrected water/fat 3D grey-blood phase sensitive inversion recovery (PSIR) late gadolinium enhancement (LGE) technique has shown excellent agreement with 2D grey-blood LGE MRI [1], while providing higher spatial resolution and coverage, and complementary fat volumes [2]. This approach was previously evaluated after bolus injection at an isotropic resolution of 2mm3, correcting only for 2D translational respiratory motion, with a scan time of ~10 min. However, contrast washout may impact scar detection [3] and limit spatial resolution [4] due to the relative long scan time. In this study, we sought to investigate the proposed water/fat 3D grey-blood PSIR LGE MRI in combination with 3x undersampling and non-rigid motion-corrected reconstruction [5] and higher isotropic spatial resolution acquired after slow infusion. We compared the slow-infusion approach against the previously evaluated bolus injection approach, using the same spatial resolution and motion-corrected reconstruction. The proposed water/fat grey-blood 3D LGE sequence was evaluated in 14 patients with suspected cardiovascular disease and compared to clinical reference 2D breath hold grey-blood PSIR LGE imaging. Qualitative and quantitative results with respect to image quality are reported.Methods
Acquisition & Reconstruction:3D water/fat LGE prototype sequence consisted of two interleaved ECG-triggered 3D volumes with a two-point Dixon encoding [6], spoiled gradient echo readout and undersampled variable-density Cartesian trajectory with spiral profile order sampling [7]. To achieve 100% respiratory scan efficiency and predictable scan time, image navigators (iNAVs) [8] are acquired at each heartbeat immediately preceding the 3D readout. In the first volume, data is acquired with an IR pulse preceding the imaging sequence with patient specific inversion time set to null the blood signal, whereas the second volume is acquired with no preparation pulses. Beat-to-beat 2D translational respiratory motion correction is estimated in foot-head and left-right from the 2D iNAVs and applied to all four echoes. 3D non-rigid motion is estimated from respiratory bin images and incorporated into a motion-compensated reconstruction with patch-based low-rank regularization [9] for all 4 echoes. To generate the water/fat volumes, a water/fat algorithm with magnitude based B0 estimation and phase unwrapping (B0-NICEbd) [10] was used. Polarity is restored as in work by Milotta et al [2].
Imaging & Analysis:
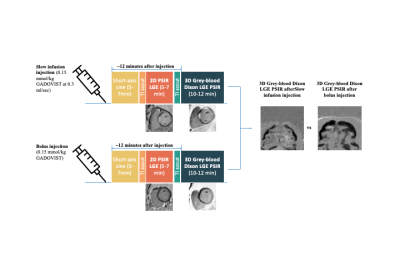
The water/fat grey-blood 3D PSIR LGE protocol was evaluated in 14 patients with suspected cardiovascular disease in comparison to the clinical reference 2D breath hold grey-blood PSIR LGE imaging at 1.5T (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany). Seven patients (6 males, 57±14yo) underwent 3D LGE after slow infusion and seven patients (6 males, 53±13yo) underwent 3D LGE after bolus injection. Acquisitions were performed on a 1.5T scanner (Siemens Magneton Aera) with the following imaging parameters: coronal orientation, FOV=320x320x132-144mm, resolution=1.5mm3, bandwidth=600Hz/px, TR/TE1/TE2=6.41/2.38/4.76ms, FA=25° and 5° for IR prepared and non-prepared volumes, 14 echoes for iNAV acquisition with FA=3°. Clinical reference 2D PSIR LGE images (imaging parameters: FA=45˚, resolution=2x2x8mm, breath-hold per slice=12s, 16–18 slices) were acquired 5-7 min after contrast injection of 0.15mmol/kg (Gadovist), whereas 3D LGE sequences were acquired ~12 min after contrast injection (Fig.1). Slow infusion was performed at a rate of 0.3ml/s. Proposed water/fat grey-blood 3D PSIR LGE with slow infusion was compared against water/fat grey-blood 3D PSIR LGE after bolus injection and clinical reference 2D PSIR LGE. Image quality was ranked by a clinical expert (4-point Likert scale (1: non-diagnostic, 4: excellent diagnostic quality).
Results
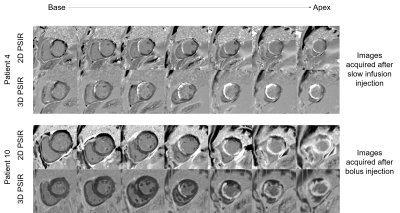
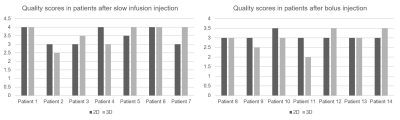
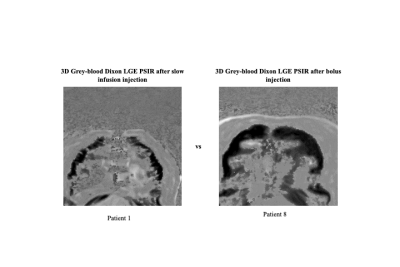
Comparison of the 2D grey-blood PSIR and 3D grey-blood PSIR images in short axis, 2 chamber and 4 chamber views are shown in Fig.2 for a representative patient with slow infusion and one with bolus injection. Comparison of 2D grey-blood and 3D grey-blood PSIR images for several short-axis slices is shown in Fig.3 for two additional patients. Good agreement and depiction of scar is observed with the proposed 3D LGE sequence with both contrast injection administrations, in comparison to 2D LGE, while improving the volumetric coverage and avoiding repeated breath-holding. Image quality assessment is shown in Fig.4. Slightly lower image quality scores can be observed in patients P2, P4, P9 and P11 with 3D PSIR LGE due to remaining water/fat swaps (P2, P9) and motion artefacts (P4 and P11). Improved image quality and easier visualisation of the scar due to the better coverage in the 3D grey-blood PSIR images was observed in five patients. Overall image quality was rated better in cases acquired after the slow infusion injection. 3D grey-blood PSIR volumes for both contrast administrations are also shown in Fig.5 for further comparison.Conclusion
The proposed high-resolution 3D grey-blood PSIR slow infusion protocol has been successfully tested in seven patients imaged after slow infusion injection and seven patients after bolus injection enabling scar visualisation in water PSIR volume while also providing high-resolution fat images. Comparable image quality was observed between the 2D PSIR LGE and 3D PSIR LGE images. Overall, images acquired after slow infusion resulted in better quality score than images acquired after bolus injection. Future work will include investigating this protocol in a larger cohort of patients.Acknowledgements
This work was supported by EPSRC (EP/L015226/1, EP/P032311/1, EP/P007619/1 and EP/P001009/1) and the Wellcome/EPSRC Centre for Medical Engineering (NS/A000049/1).
References
[1] Holtackers RJ, Chiribiri A, Schneider T, Higgins DM, Botnar RM. Dark-blood late gadolinium enhancement without additional magnetization preparation. J Cardiovasc Magn Reson 2017;19. https://doi.org/10.1186/S12968-017-0372-4.
[2] Milotta G, Munoz C, Kunze K, Neji R, Figliozzi S, Masci P, et al. 3D Whole-heart Motion Compensated Grey-blood Late Gadolinium Enhancement Imaging. ISMRM 2020:Abstract 2045. https://cds.ismrm.org/protected/20MPresentations/abstracts/2045.html (accessed December 15, 2020).
[3] Munoz C, Bustin A, Neji R, Kunze KP, Forman C, Schmidt M, et al. Motion-corrected 3D whole-heart water-fat high-resolution late gadolinium enhancement cardiovascular magnetic resonance imaging. J Cardiovasc Magn Reson 2020;22:53. https://doi.org/10.1186/s12968-020-00649-5.
[4] Bi X, Carr JC, Li D. Whole-heart coronary magnetic resonance angiography at 3 Tesla in 5 minutes with slow infusion of Gd-BOPTA, a high-relaxivity clinical contrast agent. Magn Reson Med 2007;58:1–7. https://doi.org/10.1002/mrm.21224.
[5] Cruz G, Atkinson D, Henningsson M, Botnar RM, Prieto C. Highly efficient nonrigid motion-corrected 3D whole-heart coronary vessel wall imaging. Magn Reson Med 2017;77:1894–908. https://doi.org/10.1002/mrm.26274.
[6] Foley JRJ, Fent GJ, Garg P, Broadbent DA, Dobson LE, Chew PG, et al. Feasibility study of a single breath-hold, 3D mDIXON pulse sequence for late gadolinium enhancement imaging of ischemic scar. J Magn Reson Imaging 2019;49:1437–45. https://doi.org/10.1002/jmri.26519.
[7] Prieto C, Doneva M, Usman M, Henningsson M, Greil G, Schaeffter T, et al. Highly efficient respiratory motion compensated free-breathing coronary mra using golden-step Cartesian acquisition. J Magn Reson Imaging 2015;41:738–46. https://doi.org/10.1002/jmri.24602.
[8] Henningsson M, Koken P, Stehning C, Razavi R, Prieto C, Botnar RM. Whole-heart coronary MR angiography with 2D self-navigated image reconstruction. Magn Reson Med 2012;67:437–45. https://doi.org/10.1002/mrm.23027.
[9] Bustin A, Milotta G, Ismail TF, Neji R, Botnar RM, Prieto C, et al. Accelerated free-breathing whole-heart 3D T2 mapping with high isotropic resolution. Magn Reson Med 2019;83:988–1002. https://doi.org/10.1002/mrm.27989.
[10] Liu J, Peters DC, Drangova M. Method of B0 mapping with magnitude-based correction for bipolar two-point Dixon cardiac MRI. Magn Reson Med 2017;78:1862–9. https://doi.org/10.1002/mrm.26569.
Figures