1562
Evaluation of non-contrast free-breathing compressed SENSE T1-TFE cardiac MRI at 3T in young children with congenital heart diseases1Department of Diagnostic and Interventional Radiology and Nuclear Medicine, University Medical Center Hamburg-Eppendorf, Hamburg, Germany, 2Philips GmbH Market DACH, Hamburg, Germany, 3Department of Diagnostic and Interventional Radiology and Nuclear Medicine, Section of Pediatric Radiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany, 4Institute of Medical Biometry and Epidemiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany, 5University Heart Center, Adult Congenital Heart Disease Unit, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
Synopsis
High-quality cardiac MRI at 3T in sedated children with congenital heart disease (CHD) is challenging, because of field inhomogeneities and free breathing motions. Therefore, we aimed to employ the non-contrast free-breathing generic T1-weighted turbo-field echo (TFE) sequence with compressed sensing reconstruction for assessment of vessel diameters and evaluation of the intra- and extracardiac structures in children with CHD aged <5 years. Our results show a highly reliable clinical applicability for intra- and extracardiac structures with significantly higher accuracy in comparison to contrast-enhanced MR-angiography and 3D-Dixon sequences.
Introduction
Magnetic resonance imaging of the heart is considered a valuable clinical tool for studying congenital heart disease (CHD) in children and adults1,2. However, simple, high-quality imaging in young children is challenging due to respiratory motions. On the other hand, imaging at high field poses extra challenges to the balanced SSFP contrast caused by susceptibility differences or field inhomogeneities, especially with 3T scanners. We aimed to employ the generic free-breathing T1-weighted turbo-field echo (TFE) sequence with compressed sensing reconstruction for assessment of vessel diameters and evaluation of the intra- and extracardiac structures in pediatric patients <5 years with CHD.Methods
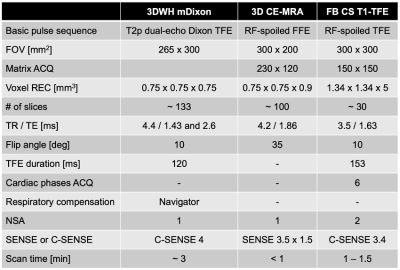
37 children with CHD (20 male, mean age 1.5 years ± SD 1.4, range: 0-4) have been examined by cardiac MRI at 3.0T using a standard 32-channel torso coil (Ingenia, Philips Healthcare, Best, the Netherlands) with 70 cm bore between 2018 – 2020. They were retrospectively included in this single center study. The following sequences were applied: 1) Non-contrast free-breathing cine scans based on T1-weighted turbo-field echo sequences (FB CS T1-TFE), 2) 3D whole-heart modified Dixon imaging3 (3D WH-mDixon), and 3) contrast-enhanced MR-angiography (3D CE-MRA). For free-breathing pseudo-cine imaging, the generic radiofrequency (RF) spoiled SSFP was applied to destroy the residual transverse magnetization at the end of each repetition time (TR), which creates a T1-weighted contrast4,5. Scan parameters were optimized for adequate spatial resolution and signal strength. Multiple signal averages (NSA) were performed helping to average out the bulk motion effect to a certain degree and improve SNR in general. The recently introduced compressed SENSE technique6,7, which employed compressed sensing together with coil sensitivity information, was used to shorten the scan time. Detailed parameters are summarized in Fig. 1. Two attending radiologists independently assessed 1) overall image quality and 2) quality of different vessels of interest (ascending aorta; supra-aortic vessels; pulmonary arteries; superior and inferior vena cava; pulmonary veins) in each of the three sequences (3D WH-mDixon; 3D CE-MRA; FB CS T1-TFE) on a five-point Likert scale (1= non-diagnostic image quality; 5= excellent image quality). Moreover, diagnostic confidence for detection or exclusion of pathologies was rated on a five‑point Likert scale (1= very unsure; 5= highly confident). For quantitative evaluation, diameters of the aorta and pulmonary artery were measured at seven predefined anatomic landmarks. Friedmann-ANOVA was performed to test for statistical differences regarding image quality and diagnostic reliability followed by Wilcoxon-Test to determine their directionality based on pairwise comparisons. Krippendorff's alpha (0= no reliability; 1= perfect reliability) was calculated to determine the agreement between the two readers regarding diameter measurements for each sequence.Results and Discussion
Representative images of patients with extracardiac vessel abnormalities are displayed in Fig. 2, whereas Fig. 3 depicts images of patients with intracardiac pathologies. Overall image quality ratings showed statistically significant effects for all items examined (Friedmann ANOVA all p< 0.001). Wilcoxon post-hoc tests revealed significantly superior overall image quality as well as diagnostic confidence (Fig. 4) for FB CS T1-TFE. Compared with the other two sequences, FB CS T1-TFE was consistently associated with higher Krippendorff's alpha values and thus indicated better agreement with respect to vascular diameter measurements between both readers (exception: approximately equivalent result with respect to the ascending aorta in 3D WH-mDixon, Fig. 5). 14.5 % (90 out of 620) of the vessels analyzed in the 3D WH-mDixon and 3.6 % (20 out of 560) analyzed in the 3D CE-MRA could not be quantified reliably due to poor image quality, whereas diameters for all vascular structures (740 out of 740) could be measured in the FB CS T1-TFE by both readers. In summary, FB CS T1-TFE results in consistent high contrast image quality with sharp delineation of both intracardiac and extracardiac structures which leads to a significantly higher diagnostic confidence as well as agreement for quantitative measurements.Conclusion
In contrast to 3D CE-MRA and 3D WH-mDixon, non-contrast free-breathing T1-TFE based on generic RF spoiling and compressed SENSE reconstruction demonstrated to be a robust sequence at 3T with higher image quality and diagnostic confidence in sedated pediatric CHD patients <5 years in this preliminary single center study. However, further systematic investigations are warranted to evaluate accuracy for various pathologies in comparison to clinical standard of care.Acknowledgements
No acknowledgement found.References
1. Fratz S, Chung T, Greil GF, et al. Guidelines and protocols for cardiovascular magnetic resonance in children and adults with congenital heart disease: SCMR expert consensus group on congenital heart disease. J Cardiovasc Magn Reson. 2013;15:512.
2. Ntsinjana HN, Hughes ML, Taylor AM. The Role of Cardiovascular Magnetic Resonance in Pediatric Congenital Heart Disease. J Cardiovasc Magn Reson. 2011;13:51.3.
3. Kourtidou S, Jones MR, Moore RA, et al. mDixon ECG-gated 3-dimensional cardiovascular magnetic resonance angiography in patients with congenital cardiovascular disease. J Cardiovasc Magn Reson 2019;21:52.4.
4. Frahm J, Haase A, Mattaei D. Rapid NMR imaging of dynamic processes using the FLASII technique. Magn Reson Med 1986;3:321-327.5.
5. Zhang S, Block KT, Frahm J. Magnetic resonance imaging in real time: advances using radial FLASH. J Magn Reson Imaging 2010;31:101.6.
6. Schoennagel BP, Yamamura J, Kording F, et al Fetal dynamic phase-contrast MR angiography using ultrasound gating and comparison with Doppler ultrasound measurements. Eur Radiol (2019) 29:4169.7.
7. Salehi D, Sun L, Steding-Ehrenborg K, et al. Quantification of blood flow in the fetus with cardiovascular magnetic resonance imaging using Doppler ultrasound gating: validation against metric optimized gating. J Cardiovasc Magn Reson (2019) 21:74.
Figures

Intraindividual comparison of all three sequences (from left to right) in three different patients. FB CS T1-TFE demonstrated highest contrast resulting in sharp delineation of various extracardiac structures.
A) 3-month-old boy with an hypoplastic aortic arch (arrowhead). Asterisk indicates the main pulmonary artery.
B) 3-year-old boy with a partial anomalous pulmonary venous connection to superior vena cava (arrowhead).
C) 3-year-old girl with a persistent left superior vena cava (arrowhead).
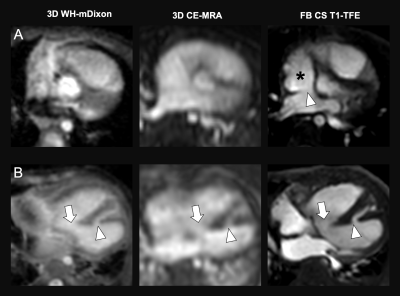
Intraindividual comparison of all three sequences (from left to right) in two different patients. FB CS T1-TFE demonstrated superior image contrast for sharp delineation of intracardiac structures.
A) 3-year-old female patient with an atrial septal defect (arrowhead). Asterisk indicates the right atrium.
B) 3-month-old male patient with two ventricular septal defects (arrow + arrowhead).

A) Descriptive statistics (left) displays mean (M) vessel quality scores (Likert scale 1-5) and standard deviations (SD) of both readers. Statistical analysis (right) revealed significantly better image quality in FB CS T1-TFE for all items tested. R1: Reader 1, R2: Reader 2.
B) Box-plots display the distribution of the readers´ quality ratings with FB CS T1-TFE achieving highest scores. SupraAo: Supra-aortic vessels, MPA: Main pulmonary artery, L/RPA: left/right pulmonary artery, VCI: inferior vena cava, VCS: superior vena cava, PuVeins: pulmonary veins.
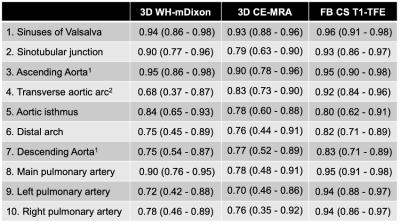
Vessel diameter measurement agreement between the two readers.
Krippendorff's alpha (0= no reliability, 1= perfect reliability) indicates agreement for diameters at 7 predefined anatomic landmarks of the aorta (1.-7.) and pulmonary arteries (8.-10.). 1Diameter was assessed at the level of main pulmonary trunc; 2Diameter was assessed between brachiocephalic trunc and left common carotid artery.