1557
Contrast-free 3D Cartesian MRA of the thoracic aorta in 3 min: preliminary clinical evaluation11School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom, 2Guy's and St Thomas' Hospital, London, United Kingdom, 3MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom, 42MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom, 5Escuela de Ingeniería, Pontificia Universidad Católica de Chile, Santiago, Chile
Synopsis
Cardiovascular Magnetic Resonance Angiography is established for serial monitoring of thoracic aortic disease. Limitations of the current approach include the diaphragmatic navigation, leading to long acquisition times and the correction of the aortic motion, solely in one direction. We propose a T2-prep bSSFP sequence that incorporates image-based navigation and inline non-rigid motion-correction for efficient, free-breathing and isotropic aortic imaging. Comparison between the conventional and the research sequence shows similar diagnostic confidence with both techniques in much shorter acquisition time [3.11.1min (iNAV) versus 11.5 min3.4 (dNAV),P<0.0001] and good agreement of aortic measurements between both techniques, holding promise for forthcoming clinical adoption.
Introduction
Cardiovascular magnetic resonance angiography (MRA) has been established for serial monitoring of thoracic aortic disease. Conventional 3D bSSFP MRA techniques use diaphragmatic respiratory gating (dNAV) to minimize the effects of respiratory motion in the images, leading to unpredictable and excessively long acquisition times along with the risk of incomplete or aborted scans because of respiratory drift. Additionally, the aortic arch experiences a wide range of displacement during the respiratory cycle1, that cannot be accurately corrected solely with the clinical dNAV approach. Here we propose to apply and evaluate the performance of a non-rigid respiratory motion compensated Cartesian coronary MRA framework previously introduced for coronary imaging2, for the visualization of the thoracic aorta in a short and predictable 3 min scan with inline reconstruction.Methods
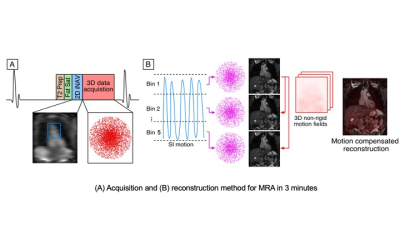
Free-breathing T2prep bSSFP sequence with image-based navigation and non-rigid motion correction provides high quality aortic imaging in approx. 3 min scan and 3 min inline reconstruction time. An ECG-triggered free-breathing 3D T2prep bSFFP sequence (Fig. 1) acquired with a 3-fold undersampled variable-density Cartesian trajectory3 is employed. 2D image navigators (iNAVs)4 are acquired at each cardiac cycle by spatially encoding the start-up echoes preceding the 3D MRA acquisition to enable 100% scan efficiency and predictable scan time (Fig 1A). The iNAVs are used to estimate foot-head and right-left (RL) rigid motion by tracking a template around the aortic arch, providing motion estimates in a beat-to-beat basis. Foot-head motion is used to sort the 3D MRA data in 5 equally populated bins, and 3D MR images reconstructed at each respiratory position are used to estimate non-rigid motion5 between bins (Fig 1B). 2D translational beat-to-beat and 3D non-rigid bin-to-bin motion is then integrated into an in-line motion-compensated iterative SENSE reconstruction to produce the final images. Imaging parameters include: FOV: 400x300x128-154 mm3, spatial resolution 1.6×1.6×1.6 mm, flip angle = 90°, T2-prep duration = 40ms, TE/TR = 1.72/3.44 ms, coronal orientation. The proposed sequence was evaluated against the clinical 3D T2prep bSSFP with dNAV gating sequence (FOV 400x300x155-165mm3, spatial resolution 1.6×1.6×1.6 mm, T2-prep duration = 40 ms, GRAPPA parallel imaging 2x undersampled, flip angle = 90˚, sagittal orientation) for the visualization of the aortic root and the thoracic aorta. Fifteen patients with thoracic aortic disease were scanned with 1.5T MRI scanner (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany). Two experts blinded to the technique used, recorded their diagnostic confidence (from 1: poor diagnostic confidence to 4: full diagnostic confidence). Co-axial aortic dimensions in three landmarks were measured by one reader with both techniques to assess agreement between the two methods. Co-axial aortic dimensions in three landmarks were measured by both readers with the proposed sequence and the second reader repeated the measurements twice, to assess inter- and intra-observer variability.Results
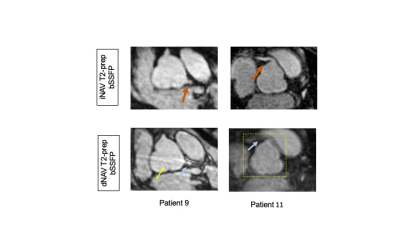
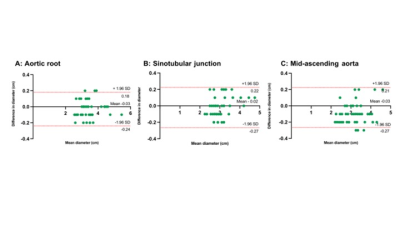
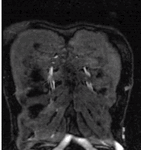
Good quality depiction of all thoracic aortic segments (Fig. 2, 3 & 5) in short scan time was achieved with the iNAV-based approach [3.1±1.1min (iNAV) versus 11.5 min±3.4 (dNAV), P<0.0001]. The reconstruction time for the proposed sequence was 3±0.3 min inline on the scanner. Diagnostic confidence was high and similar to the proposed and the clinical sequence for both reviewers (Reviewer 1: 3.80±0.41 vs 3.86±0.35, p=1; Reviewer 2: 3.86±0.35 vs 3.93±0.26,P=0.6). Bland Altman analysis showed very good agreement in the co-axial aortic measurements of the aortic root, sinotubular junction and mid-ascending aorta between the two datasets, with a small mean difference of <0.03 cm across these landmarks (Fig.3). Intraclass Correlation Coefficient showed excellent intra-observer reproducibility at the corresponding anatomic segments [aortic root (0.9; 95% CI: 0.82, 0.95), sinotubular junction (0.89; 95% CI: 0.79, 0.93), mid-ascending aorta (0.9; 95% CI: 0.81, 0.95)] and inter-observer reproducibility [aortic root (0.98; 95% CI: 1, 1), sinotubular junction (0.99; 95% CI: 1, 1), mid-ascending aorta (0.99; 95% CI: 1, 1)].Discussion
The 2D image-based navigation allows the extraction of the position of the aortic arch during the respiratory cycle directly from the data, accepting data all respiratory positions and leading to a significant acceleration of the acquisition time compared to conventional diaphragmatic navigation. Additionally the non-rigid motion correction can resolve the aortic shift during the respiratory and cardiac cycle efficiently. This has been shown to be significant in some subjects, for whom the motion at the ascending aorta is greater than that at the aortic arch and the descending thoracic aorta5,6, improving the delineation of the aortic segments despite the faster acquisition time. The proposed respiratory-motion compensation and reconstruction approach offers a novel framework for sharp aortic imaging in fast scan time.Conclusion
Thoracic aortic iNAV-based MRA provided high quality visualisation of the thoracic aorta in a cohort of patients with thoracic aortic disease, in shorter and more consistent scan times than the current clinical standard. High diagnostic confidence, reproducible aortic measurements and fast inline reconstruction are promising for imminent clinical integration.Acknowledgements
No acknowledgement found.References
1. Sailer AM et al. Journal of Endovascular Therapy. 2015;22(6):905-911.
2. Cruz G et al. Magn Reson Med. 2017;77(5):1894.
3. Prieto C. et al. J Magn Reson Imaging 41:738–746.
4. Henningsson M et al. Magn Reson Med. 2012;67:437- 445. 5. Bustin A. et al, J Cardiovasc Magn Reson. 2020;22(1).
5. Weber TF et al. Cardiovasc Intervent Radiol. 2009.
6. Suh GY et al. J Vasc Interv Radiol. 2014.
Figures