1555
One-stop subtractionless first-pass CS-whole-body MRA with once contrast injection of 0.15mmol/kg dose: first clinical experience
Qing FU1, Jia-wei Wu1, Jing-yang Li1, Peng Sun2, and Xiang-chuang Kong1
1Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China, 2Philips Healthcare, Beijing, China
1Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China, 2Philips Healthcare, Beijing, China
Synopsis
Conventional subtracted whole-body CE-MRA is time-consuming and requires experiences for operators. Instead, one-stop subtractionless CS-MRA in our study could depict the whole-body arterial vasculatures with only once contrast injection and only 0.15 mmol/kg dose, which assisted by multiple techniques including reverse k-space filling mode, total imaging matrix system, automatic table moving, automatic coil selection and especially the CS technique. The comparative results supported it feasible with accepted image qualities and a faster acquisition time in clinical use.
Purpose
To investigate the feasibility and clinical utility of a subtractionless compressed sensing (CS) whole-body MRA protocol by using two-point Dixon fat suppression and only once first-pass contrast injection with only 0.15mmol/kg dose for suspected peripheral vascular disease (PVD) in comparison to conventional subtraction MRA.Materials and Methods
This study was approved by the local institutional review board. MR examinations were performed with a 3.0T MR scanner (Ingenia CX, Philips Healthcare). A 20-channel head-neck coil and two 32-channel array coils were used for coverage from head vertex to ankle level. From Sep 2020 to Oct 2021, 9 healthy volunteers (3 male,6 female, 40.0 ±15.5 years old) with no history of symptoms of arterial diseases were enrolled to perform conventional subtraction CE-MRA, and 47 patients with clinical suspected PVD (23 male,24 female, 55.9 ± 16.4 years old) were enrolled to perform subtractionless CS-MRA protocol. The Whole-body CE-MRA images were acquired with 3D pulse sequences in a successive order based on acquisitions of 5 overlapped stations: station I (head-neck), station II (thorax-abdomen), station III (abdomen-pelvis), station IV (upper leg), and station V (lower leg). In CS-MRA protocol, MRA was obtained using CS and parallel imaging accelerated two-point DIXON fat suppression without the need for pre-post-subtraction, detailed parameters were listed in Table 1. Only once first-pass contrast injection was applied, and the detailed injection strategy was listed as follows: a single dose (0.1mmol/kg) contrast was injected at a flow rate of 2.0ml/s, then followed by a half dose (0.05mmol/kg) at a flow rate of 1.0ml/s, and finally, followed by a saline bolus 15ml at a flow rate of 1.0ml/s. In conventional MRA protocol, MRA was subtracted from pre-and post-images using fast field echo 3D sequence (FFE), detailed parameters were listed in Table 2. Contrast material was injected with a biphasic injection strategy, the first injection was used for imaging coverage from the thorax-abdomen-pelvis-upper leg-lower leg, 0.1mmol/kg contrast was injected at a flow rate of 2.0 ml/s, then 0.05mmol/kg contrast was injected at a flow rate of 1.0ml/s, finally followed by a 15ml saline bolus at a rate of 1.0ml/s. Then five minutes later, the second injection was used for imaging the head-neck area, 0.15mmol/kg contrast was injected at a rate of 2.5ml/s, followed by a 15ml saline bolus at a rate of 2.5ml/s.Objective analysis: SNRs and CNRs of the two MRA groups on four segments (common carotid arteries, abdominal aorta, common femoral arteries, and popliteal arteries) were measured and compared. SNR=SIvessel/SD, CNR=(SIvessel-SIbackground)/SD.
Subjective analysis: For image analysis, the arterial tree was divided into 36 vessel segments. The overall image quality of CS-MRA dataset and visualization of each arterial segment was evaluated by two observers in consensus using a 4-point scoring scale, image quality was rated as accepted diagnostic level only if score >=3; venous enhancement contamination was rated using a 3-point scale (Table 3).
Statistical analysis: SPSS software was used. SNR and CNR were compared by independent t test or Wilcoxon signed-rank test. A p-value < 0.05 was considered statistically significant.
Results
All examinations were finished without any adverse reactions. The cumulative scanning time of CS-MRA sequences was 60.4s, it was 193.8s for conventional subtraction MRA.Total 1739 segments were analyzed in this study, in which total 17 segments were excluded from analyses due to failure of image reconstruction, resulting in a total number of 1722 arterial segments were available for evaluation. For the subjective evaluation, 99.1% (1707/1722) of the vessel segments were rated as accepted diagnostic level with score 3-4, while 15 vessel segments were rated as only score 1-2; and 7 vessel segments were contaminated severely by venous enhancement (score 3), the other 99.6% (1715/1722) vessel segments showed minimal to moderate venous enhancement (Fig 1 and 2).
There were no significant differences in SNRs and CNRs of common carotid arteries, common femoral arteries, and popliteal arteries between the two groups (all p>0.05). The SNR and CNR of the abdominal aorta in CS-MRA were both inferior to that of the conventional MRA group (p=0.017 and p=0.036, respectively).
Discussion and Conclusion
Multiple techniques including reverse k-space filling mode, total imaging matrix system, automatic table moving, automatic coil selection techniques and especially the CS help the fast acquisition of each station of the whole-body-MRA imaging, making the once contrast injection strategy possible. Because the arterial time window between station I and II is very short, two techniques were applied to make it possible for once injection. First, central part of k-space was filled last (rev-CENTRA), and then central part of k-space was filled first in station II. Second, scan time of station I was adjusted to only 9.8s. The two-point DIXON water-fat separation can suppress fat signals with no need of subtraction, avoiding the possibility of misregistration artefact caused by patient motion and thus improve vasculature conspicuity. Even though SNRabdominal aorta and CNRabdominal aorta of CS-MRA were inferior to those of conventional MRA, subjective scores analysis supported the accepted diagnostic level for the CS-MRA protocol.This study demonstrated that one-stop subtractionless CS-whole body-MRA protocol could provide excellent image quality for fist-pass whole-body arterial vasculature compared with conventional subtraction-based CE-MRA method, and allowing a faster whole-body MRA workflow in clinical use.
Acknowledgements
noneReferences
1. Nael K, Ruehm SG, Michaely HJ, et al (2007) Multistation Whole-Body High-Spatial-Resolution MR Angiography Using a 32-Channel MR System. American Journal of Roentgenology 188:529–539. https://doi.org/10.2214/AJR.05.20532. Fenchel M, Requardt M, Tomaschko K, et al (2005) Whole-body MR angiography using a novel 32-receiving-channel MR system with surface coil technology: First clinical experience. J Magn Reson Imaging 21:596–603. https://doi.org/10.1002/jmri.203033. Leiner T, Habets J, Versluis B, et al (2013) Subtractionless first-pass single contrast medium dose peripheral MR angiography using two-point Dixon fat suppression. Eur Radiol 23:2228–2235. https://doi.org/10.1007/s00330-013-2833-yFigures

Figure 1: A: Whole-body MRA MIP of a female healthy volunteer (47 years old) by conventional subtracted-MRA; B: Whole-body MRA MIP of another healthy volunteer (male, 50 years old) by subtractionless CS-MRA, showing excellent image quality to depict the whole-body arterial vessels.

Figure 2: Patient, male, 78 years old, suffered from arteriosclerosis obliterans of lower extremities accompanied by gangrene. Subtractionless CS-MRA showed that, left internal carotid artery, left femoral and popliteal arteries had complete occlusion; bilateral calf arteries had severe stenoses, accompanied by multiple collateral circulation with small vessels; right internal and external carotid arteries, bilateral internal iliac arteries had moderate-severe stenoses.
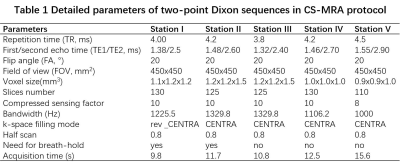
Table 1
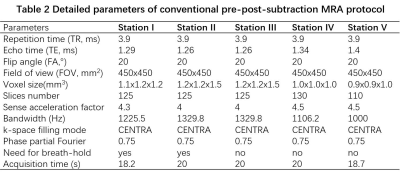
Table 2
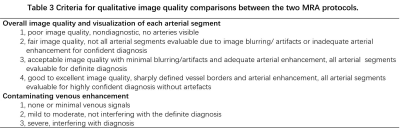
Table 3
DOI: https://doi.org/10.58530/2022/1555