1550
Post-traumatic stress disorder may affect the progression of cognitive impairment in World Trade Center responders1Biomedical Engineering, Stony Brook University, Stony Brook, NY, United States, 2Program in Public Health, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States, 3Department of Family, Population, and Preventive Medicine, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States, 4Department of Radiology, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States, 5Department of Psychiatry, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States, 6Department of Environmental Medicine and Public Health, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 7Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 8Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 9Stony Brook World Trade Center Wellness Program, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States, 10Department of Medicine, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States
Synopsis
A larger than expected number of World Trade Center (WTC) responders, now at midlife, are experiencing chronic post-traumatic stress disorder (PTSD) and incidence of mild cognitive impairment (MCI). A previous study reported that WTC responders with MCI have altered white matter connectivity when compared to unimpaired responders. However, the effects of PTSD on fiber integrity in this population was not studied due to a limited sample size. In the present study, we analyzed 97 WTC responders with/without CI and/or PTSD. Our results suggest that PTSD may influence the neuropathology of CI within this population.
Introduction
In the aftermath of the terrorist attacks on September 11, 2001, World Trade Center (WTC) responders were emotionally, mentally, and physically exposed to extreme conditions during search-and-rescue operations. In the two decades since, it is estimated that 23% of these responders present with chronic post-traumatic stress disorder (PTSD)1,2,3. Studies in other populations report changes in white matter integrity in patients diagnosed with PTSD4.Responders diagnosed with WTC-related PTSD have a higher incidence of mild cognitive impairment (MCI)5, a precursor to Alzheimer’s disease (AD). Recently, it was reported that white-matter connectivity is altered in WTC responders diagnosed with MCI when compared to cognitively unimpaired (CU) subjects6. Whether or not the MCI responders’ tract integrity is impacted by PTSD was not studied due to limited sample size and has yet to be investigated. In this work, we analyzed diffusion data of 97 WTC responders to identify the affected tracts of cognitively impaired (CI) and CU subjects with or without PTSD. Our results suggest PTSD potentially influences the neuropathology of CI.
Methods
Ninety-seven subjects were included in this study, 49 of which were CI. Responders were identified as CI or CU using the Montreal Cognitive Assessment (MoCA). A conservative cutoff at a level consistent with possible mild dementia (MoCA ≤ 20) was used to determine CI status. CU controls had scores in the normal range (MoCA > 26). All subjects were scanned on the same 3T Siemens Biograph mMR with diffusion acquisition parameters: TE/TR = 87.6/4680 ms, b value = 1000, 64 diffusion directions, in-plane resolution = 2×2 mm2, slice thickness = 2 mm, matrix size = 128×128, multiband factor = 2.Two analyses were performed to study: (1) CI vs. CU in responders without PTSD (CI/PTSD- vs. CU/PTSD-, N = 25, 24, respectively) and (2) CI vs. CU in responders with PTSD (CI/PTSD+ vs. CU/PTSD+, N = 24, 24, respectively). The sample distribution is summarized in Table 1. Connectometry analyses were performed using DSI Studio, a tractography software used to track fiber bundles7. The t-score threshold was set to t = 2.5. Diffusion MRI connectometry was used to derive the correlational tractography that has FA values correlated with the study variable with age/sex correction.
Results
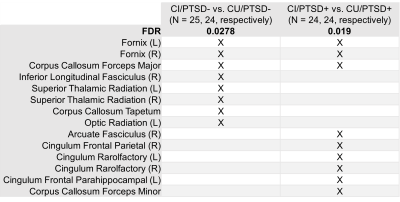
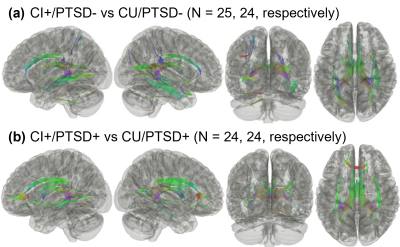
Table 2 summarizes the white matter bundles with reduced connectivity for the two analyses. In responders without PTSD, CI subjects have reduced white matter connectivity in eight white matter tract bundles when compared to their CU counterparts. These regions are predominantly localized in the limbic system.Among responders with PTSD, the ones with CI exhibit nine bundles with decreased FA, compared to their CU counterparts. These tract bundles are also mainly confined to the limbic system, particularly along the cingulum. The spatial distribution of the affected tracts is shown in Fig. 1.
As shown in Table 2, CI affects white matter connectivity differently in the responders with and without PTSD.
Discussion
As illustrated in Fig. 1a, when comparing responders without PTSD, the majority of altered white matter tracts of subjects with CI are localized within the limbic system. This finding is consistent with the literature, as abnormalities in the limbic pathway is associated with CI in multiple sclerosis8, Parkinson’s disease9, and AD10.In contrast to CU responders with PTSD, individuals with both PTSD and CI also present with reduced connectivity in the limbic system, regions along the cingulum bundle also present with decreased FA. The reduced connectivity is asymmetrically distributed along the cingulate tract, agreeing with the literature11.
As shown in Table 2, the two analyses identified a few common bundles. However, there were also distinct bundles to each analysis. This finding supports the hypothesis that PTSD may potentially influence the pathology of CI among WTC responders.
Conclusion
Our findings indicate that there are distinct white matter bundles affected by CI among responders with PTSD and without PTSD. This finding suggests that PTSD may alter the progression of CI in the WTC responder cohort.Acknowledgements
This works was supported by the National Institutes of Health (NIH/NIA R01 AG049953), the Centers for Disease Control and Prevention (CDC/NIOSH 200-2011-39361). We would like to acknowledge and kindly thank all the participant WTC responders in this study and Ms. Melissa Carr for her supervision and coordination of participant recruitment.References
1. Azofeifa, A. et al. World Trade Center Health Program—United States, 2012− 2020. MMWR Surveillance Summaries. 2021. 70(4):1.
2. Bromet, E. J., et al. DSM-IV post-traumatic stress disorder among World Trade Center responders 11–13 years after the disaster of 11 September 2001 (9/11). Psycho. Med. 2016. 46(4):771-783.
3. Giesinger, I., et al. Association between posttraumatic stress disorder and mortality among responders and civilians following the September 11, 2001, disaster. 2020. JAMA Netw. Open. 3(2):e1920476-e1920476.
4. Daniels, J. K., et al. White matter integrity and its relationship to PTSD and childhood trauma—A systematic review and meta‐analysis. Depress. Anxiety. 2013. 30(3):207-216.
5. Clouston, S. A., et al. Incidence of mild cognitive impairment in World Trade Center responders: long‐term consequences of re‐experiencing the events on 9/11/2001. Alzheimer's Dement. (Amst). 2019. 11(1):628-636.
6. Huang, C., et al. White Matter Connectivity in Incident Mild Cognitive Impairment: A Diffusion Spectrum Imaging Study of World Trade Center Responders at Midlife. J. Alzheimer’s Dis. 2021. 80(3):1209-1219
7. Yeh, F. C., Badre, D. and Verstynen, T. Connectometry: a statistical approach harnessing the analytical potential of the local connectome. Neuroimage. 2016. 125:162-171.
8. Keser, Z. et al. Limbic pathway correlates of cognitive impairment in multiple sclerosis. J. Neuroimaging. 2017. 27(1):37-42.
9. Gao, Y., et al. Changes of brain structure in Parkinson’s disease patients with mild cognitive impairment analyzed via VBM technology. Neurosci. Lett. 2017. 658:121-132.
10. Nestor, P. J., et al. Limbic hypometabolism in Alzheimer's disease and mild cognitive impairment. Ann. Neurol. 2003. 54(3):343-351.
11. Kim, S. J., et al. Asymmetrically altered integrity of cingulum bundle in posttraumatic stress disorder. Neuropsychobiology. 2006. 54(2):120-125.Figures
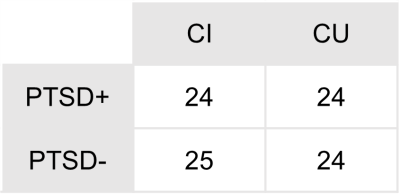
Table 1. The distribution of subjects between the
divided groups is summarized.
CI:
cognitively impaired
CU:
cognitively unimpaired