1477
Dark Blood, Susceptibility-Insensitive 3D Unbalanced Steady-State Free Precession: A Potential New Approach for Lung Cancer Screening1Radiology, NorthShore University HealthSystem, Evanston, IL, United States, 2Radiology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States, 3Siemens Medical Solutions USA, Chicago, IL, United States, 4Radiology, Pritzker School of Medicine, University of Chicago, Chicago, IL, United States
Synopsis
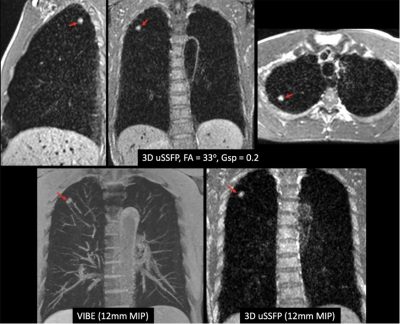
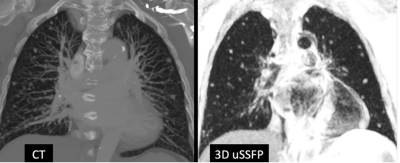
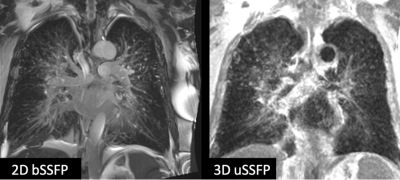
We recently described the feasibility of using a prototype 3D unbalanced steady-state free precession (3D uSSFP) pulse sequence for dark blood imaging. We sought to determine whether this technique could be adapted for dark blood, susceptibility-insensitive imaging of the lungs. A breath-hold, ECG-gated version of 3D uSSFP was implemented for a pilot study of healthy volunteers and patients. Initial results suggest that 3D uSSFP allows efficient volumetric imaging of the lungs and can demonstrate even small lung nodules without artifacts. With further development, the technique could provide a radiation-free alternative to low-dose CT for lung cancer screening.
INTRODUCTION
Over the past two decades, there has been growing interest in using non-contrast low dose computed tomography (LDCT) to screen high-risk individuals for lung cancer. Annual screening with LDCT reduces lung cancer-specific mortality by as much as 20% compared with chest radiography1. However, LDCT has several drawbacks. For instance, it provides only a very limited capability to characterize pulmonary nodules, relying primarily on lesion size to determine malignant potential. The low specificity in conjunction with the frequent occurrence of incidental findings (up to 20% of LDCT exams) often leads to biopsy or additional imaging tests such as PET-CT, increasing medical costs and subjecting the patient to unwanted stress and risk. Moreover, for centrally located lesions, the lack of vessel enhancement on a non-contrast exam can make it difficult to confidently distinguish between pulmonary nodules and vascular structures. Magnetic resonance imaging (MRI) provides a potential alternative to LDCT for the evaluation of pulmonary nodules2. Neoplasms can be detected and characterized based on various MRI properties, including tissue relaxation times, perfusion, and the apparent diffusion coefficient. Although MRI has shown promise for the evaluation of central lung cancer and large peripheral nodules, it is considered inferior to CT and has poor accuracy for subsolid and nonsolid lesions using current imaging techniques. Challenges include spatial resolution that is lower than LDCT, respiratory motion, and susceptibility artifacts (due to the presence of air-soft tissue interfaces). Nonetheless, it has been suggested that MRI could provide a nearly equivalent life expectancy benefit as well as superior cost-effectiveness relative to LDCT3. We recently reported a novel imaging technique for dark blood imaging of the chest4. It uses a tailored 3D unbalanced steady-state free precession (3D uSSFP) pulse sequence with several features that make it uniquely attractive for non-contrast lung cancer screening, including: (i) low intravascular signal; (ii) insensitivity to off-resonance effects; and (iii) very short repetition time, providing high scan efficiency and permitting use of an ECG-gated breath-hold acquisition. We hypothesized that this technique would allow artifact-free evaluation of the lungs and permit the detection of pulmonary nodules and other lung pathology. To test this hypothesis, we evaluated 3D uSSFP in healthy volunteers and a small cohort of patients.METHODS
The study was approved by the hospital institutional review board. Imaging of 6 healthy volunteers and 6 patients with lung pathology (including sarcoid, stable benign nodule of unknown type, suspected mycobacterium avium complex, lung cancer, and pulmonary edema) was performed using a 1.5 Tesla scanner (MAGNETOM Avanto Dot, Aera, or Sola, Siemens Healthcare, Erlangen, Germany). In 2 patients, images were acquired after the administration of 0.2 mmol/kg of gadobutrol (Bayer, Berlin, Germany). In the remainder, images were acquired prior to contrast administration. Breath-hold lung imaging was performed using a prototype 3D uSSFP pulse sequence. Typical scan parameters included: TR/TE/flip angle = 1.8 ms/0.77 ms/20 - 33 degrees, slice thickness = 3 mm (interpolated to 1.5 mm), 16.7% slice oversampling, 6/8 partial Fourier along the 3D partition direction, GRAPPA acceleration factor = 2 with 64 separate reference lines, sampling bandwidth = 1838 Hz/px; shot duration = 255 ms; field of view = 400 mm. To minimize bulk motion-related dephasing, ECG gating was used to synchronize the data acquisition to the diastolic phase of the cardiac cycle. To further reduce motion sensitivity, the moment of the dephasing gradient was set to one-fifth of the moment of the readout gradient (gradient spoiler factor = 0.2). A series of 60 constant-flip-angle dummy RF repetitions was applied immediately prior to each diastolic-gated shot to drive both inflowing and in-slab spins into the steady-state. In addition to 3D uSSFP, 2D balanced steady-state free precession (bSSFP) and/or volumetric interpolated breath-hold examination (VIBE) were acquired. Images were evaluated by a single experienced observer using a 4-point scale, ranging from (1) non-diagnostic, lesion not assessable due to artifacts, to (4) excellent image quality with negligible artifacts.RESULTS
Image quality was good to excellent in all subjects. Both small and large pulmonary nodules were well shown with 3D uSSFP, as were other types of lung pathology (Figures 1 - 3). The dark blood images better distinguished pulmonary nodules from blood vessels compared with 2D bSSFP, VIBE, or non-contrast CT. Off-resonance artifacts seen with 2D bSSFP were absent with 3D uSSFP. After gadolinium administration, the blood pool appeared gray using 3D uSSFP, but still provided adequate contrast with enhancing pulmonary nodules.DISCUSSION AND CONCLUSION
Initial results suggest that 3D uSSFP allows efficient volumetric imaging of the lungs and can demonstrate even small lung nodules without artifacts. Breath-holding avoids respiratory motion artifacts, while the signal intensities of blood vessels and healthy lung tissue are suppressed by the 3D uSSFP pulse sequence providing excellent contrast with lung pathology. The use of diastolic phase ECG gating eliminates motion artifacts related to cardiac pulsation which could obscure centrally located lesions using ungated techniques such as VIBE or LDCT. With further development, 3D uSSFP could eventually provide a novel, radiation-free alternative to LDCT for lung cancer screening. It could also serve as a useful adjunctive imaging technique for cardiac MRI exams to improve the evaluation of the lungs and mediastinum, which are not well depicted using standard imaging methods.Acknowledgements
NIH grants R01 HL137920, R01 HL130093 and R01 EB027475.References
1. National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. New England Journal of Medicine. 2011 Aug 4;365(5):395-409.
2. Yu N, et al. Feasibility of pulmonary MRI for nodule detection in comparison to computed tomography. BMC Med Imaging. 2020 May 20;20(1):53. doi: 10.1186/s12880-020-00451-w.
3. Allen BD, et al. Cost-effectiveness of lung MRI in lung cancer screening. Eur Radiol. 2020 Mar;30(3):1738-1746. doi: 10.1007/s00330-019-06453-9. Epub 2019 Nov 20.
4. Edelman RR, et al. Dark blood cardiovascular magnetic resonance of the heart, great vessels, and lungs using electrocardiographic-gated three-dimensional unbalanced steady-state free precession. J Cardiovasc Magn Reson. 2021 Nov 1;23(1):127. doi: 10.1186/s12968-021-00808-2.
Figures