1476
CEST Imaging vs. DWI vs. FDG-PET/CT: Therapeutic Effect Prediction for Chemoradiotherapy in Non-Small Cell Lung Cancer Patients1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Diagnostic Radiology, Hyogo Cancer Center, Akashi, Japan, 5Radiology, Fujita Health University Hospital, Toyoake, Japan
Synopsis
We hypothesize that CEST imaging has a potential for therapeutic effect prediction in NSCLC patients treated with chemoradiotherapy and may be at least as valuable as DWI and FDG-PET/CT. Moreover, combined predictors may improve therapeutic effect prediction capability, when compared with single predictor from MRI or PET/CT. The purpose of this study was to compare the capability of therapeutic effect prediction for chemoradiotherapy among CEST imaging, DWI, FDG-PET/CT and combined predictors from MRI and PET/CT in NSCLC patients.
Introduction
In the last a few decades, FDG-PET or PET/CT and MRI including DWI and dynamic first-pass CE perfusion MRI as well as dynamic first-pass CE-perfusion CT have potentials for therapeutic effect evaluation or prediction in non-small cell lung cancer (NSCLC) patients1. On the other hands, chemical exchange saturation transfer (CEST) imaging at 3.5 ppm (APTw imaging) has been suggested as one of the MR-based molecular imaging techniques in not only brain, but also body field in the last decade. CEST Imaging can be performed on proteins, amino acids and DNAs including chemical exchangeable protons such as hydroxyl protons (-OH: ~1ppm), amine protons (-NH2: ~2ppm) and amide protons (R-C(=O)-NH2 or R-C(=O)-NHR1 <R ≠ H>: ~3.5ppm)2, 3. In addition, Ohno, et al tested the capability of APTw imaging for diagnosis of pulmonary nodule4, 5. However, no major reports have been evaluated the capability for therapeutic effect prediction among CEST, DWI and FDG-PET/CT as well as combined indexes from MRI and PET/CT in NSCLC patients treated with conservative therapy. We hypothesize that CEST imaging has a potential for therapeutic effect prediction in NSCLC patients treated with chemoradiotherapy and may be at least as valuable as DWI and FDG-PET/CT. Moreover, combined predictors may improve therapeutic effect prediction capability, when compared with single predictor from MRI or PET/CT. The purpose of this study was to compare the capability of therapeutic effect prediction for chemoradiotherapy among CEST imaging, DWI, FDG-PET/CT and combined predictors from MRI and PET/CT in NSCLC patients.Materials and Methods
Fifty stage III NSCLC patients (20 men and 30 women; ; mean age 74 years <age rang 62-81 years> underwent CEST imaging, DWI, FDG-PET/CT, and chemoradiotherapy and follow-up examinations. Based on the results of follow up examination, all patients were divided into responder (n=15) and non-responder (n=35) groups. To obtain CEST data in each subject, respiratory-synchronized FASE imaging was conducted following a series of magnetization transfer (MT) pulses. Then, magnetization transfer ratio asymmetry (MTRasym) was calculated from z-spectra in each pixel, and MTRasym map was computationally generated. To obtain radiological indexes on CEST imaging, DWI and PET/CT, ROIs were placed over each targeted lesion, and determined MTRasym, apparent diffusion coefficient (ADC) and maximum standard uptake value (SUVmax). To compare all indexes between two groups, Student’s t-test was performed. For determination of predictors for therapeutic outcome, univariate and multivariate logistic regression analyses were performed. To compare diagnostic performance among all indexes and combined predictors and determination of all feasible threshold values, ROC analyses were performed. When applied each feasible threshold value, sensitivity, specificity and accuracy were compared among all predictors and combined predictors by McNemar’s test. Finally, disease free and overall survivals between both groups assessed by each method were compared by Kaplan-Meier method followed by log-rank test. A p value less than 0.05 was considered as significant in this study.Results
Representative cases are shown in Figures 1. MTRasym, ADC and SUVmax had significant difference between responder and non-responder groups (p<0.05). Results of univariate and multivariate regression analyses for therapeutic effect prediction on CEST imaging, DWI, PET/CT and combined method are shown in Figure 2. MTRasym, ADC and SUVmax were determined as significant predictors on not only univariate, but also multi variate regression analyses (p<0.05). Results of ROC analysis for therapeutic effect prediction on CEST imaging, DWI, PET/CT and combined method are shown in Figure 3. Area under the curve, specificity and accuracy of combined predictors were significantly larger or higher than those of MTRasym or ADC as well as SUVmax (p<0.05). Results of Kaplan-Meir analysis followed by log-rank test for comparison of disease free and overall survivals are shown in Figure 4. All indexes as well as combined predictors showed significant differences of disease free and overall survivals between responders and non-responders, which were divided by feasible threshold values for all indexes (p<0.05).Conclusion
CEST is considered as at least as valuable as DWI and PET/CT and would be better to be combined all information for predicting therapeutic effect of chemoradiotherapy in NSCLC.Acknowledgements
This study was technically and financially supported by Canon Medical Systems Corporation.References
- Ciliberto M, Kishida Y, Seki S, Yoshikawa T, Ohno Y. Update of MR Imaging for Evaluation of Lung Cancer. Radiol Clin North Am. 2018;56(3):437-469.
- van Zijl PC, Yadav NN. Chemical exchange saturation transfer (CEST): what is in a name and what isn't? Magn Reson Med. 2011 Apr;65(4):927-48.
- Zhou J, Heo HY, Knutsson L, van Zijl PCM, Jiang S. APT-weighted MRI: Techniques, current neuro applications, and challenging issues. J Magn Reson Imaging. 2019;50(2):347-364.
- Ohno Y, Yui M, Koyama H, et al. Chemical Exchange Saturation Transfer MR Imaging: Preliminary Results for Differentiation of Malignant and Benign Thoracic Lesions. Radiology. 2016; 279(2): 578-589.
- Ohno Y, Kishida Y, Seki S, et al. Amide proton transfer-weighted imaging to differentiate malignant from benign pulmonary lesions: Comparison with diffusion-weighted imaging and FDG-PET/CT. J Magn Reson Imaging. 2018; 47(4): 1013-1021.
Figures
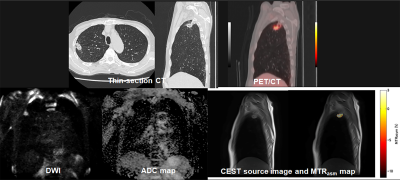
Figure 1. 62-year-old male with invasive adenocarcinoma and determined as non-responder
Thin-section CT demonstrates an invasive adenocarcinoma in the right upper lobe. SUVmax of this nodule was 2.6. ADC was 1.05×10-3mm2/s. APTw image shows low MTRasym with the value of 1.25. When applied each feasible threshold value, this case was evaluated as responder on DWI and PET/CT and non-responder on APTw image and combined predictors. Disease free survival and overall survival in this case was 18 months and 30 months.
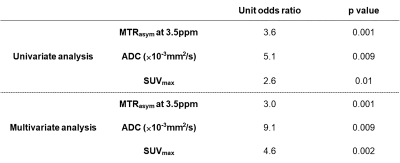
Figure 2. Results of univariate and multivariate regression analyses for therapeutic effect prediction on CEST imaging, DWI, PET/CT and combined method.
MTRasym, ADC and SUVmax were determined as significant predictors on univariate and multi variate regression analyses (p<0.05).
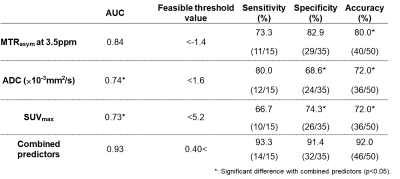
Figure 3. Results of ROC analysis for therapeutic effect prediction on CEST imaging, DWI, PET/CT and combined method.
Combined predictors showed significantly larger area under the curve than others. In addition, combined predictors also demonstrated significantly higher specificity and accuracy o than those of others (p<0.05).
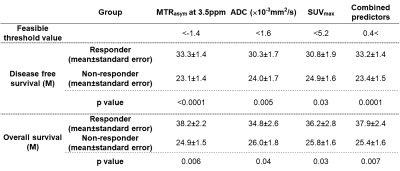
Figure 4. Results of Kaplan-Meir analysis followed by log-rank test for comparison of disease free and overall survivals.
When applied each feasible threshold value, all indexes demonstrated significant differences of disease free and overall survivals between responders and non-responders (p<0.05).