1406
Three-Dimensional real-time dynamic knee MRI using 3D cones with a multiscale low-rank reconstruction1Electrical Engineering, Stanford University, Stanford, CA, United States, 2Radiology, Stanford University, Stanford, CA, United States
Synopsis
3D real-time imaging of joints in motion can help us gain valuable insight into joint disorders. The combination of 3D golden-ratio re-ordered cones and multiscale low-rank reconstruction allow for continuous acquisition and high accelerations making 3D real time dynamic imaging of knees possible. We demonstrated the feasibility of this approach to capture patellar motion caused by a quadriceps flexion in 16 slices and with a temporal resolution of ~500ms. Although the resulting images are blurred, this method shows promise.
Introduction
Musculoskeletal (MSK) disorders are a leading source of pain globally, however, the care provided to patients with MSK disorders often has suboptimal outcomes, often due to challenges in identification of pain generators1. MSK pain and impairment is often due to improper joint loading or function. However, current imaging methods are performed in a static fashion and without dynamic loading. Disorders such as patellofemoral (PF) maltracking, require more than a standard static MRI image in order to detect the improper motion of the patella that occurs under quadriceps loading2. The diagnosis and study of these disorders could be helped by the use of real-time dynamic MRI scans. Recent developments have shown the utility real-time dynamic MSK imaging, but have been largely limited to 2D, single-slice acquisitions. The articulation of the PF joint is too complex to be viewed in a single plain or single position3 and the kinematics of the joint are dependent on position and load4. The ability to visualized 3D joint motion in real time could help us gain valuable insight into joint disorders.3D real-time imaging requires considerable acceleration of data acquisition. The combination of Parallel imaging (PI) and compressed sensing (CS) offers a solution but is limited by SNR at high acceleration factors. Recently, the data redundancy in spatiotemporal data has been exploited in cardiac and body MRI using the globally low-rank reconstruction method to achieve very high accelerations (R=19). Additionally, golden-ratio re-ordered radial acquisitions permit continuous acquisition of real-time data that can be reconstructed at various temporal resolutions. In this work we explore combining a 3D golden-ratio reordered cones sequence with a multiscale low-rank reconstruction for 3D real-time imaging of knee joint motion.
Methods
12 healthy subjects were scanned on a 3T whole-body scanner (GE SIGNA Premier) using a 16 channel receive-only phased-array flex coil. Subjects were scanned in a static position as well as during slow contraction of their quadriceps muscle at a rate of 1 hertz, to induce movement of the patella. A real-time 2D single-slice, single-shot fast-spin-echo (ssfse) sequence was acquired for reference (FOV = 16.0 cm; matrix = 200x160x1;Slice Thickness = 1 cm; TR/TE = 305/52 ms; FA = 90; Temporal resolution ~305 ms). Real-time 3D Cones was acquired utilizing a golden-ratio re-ordered acquisition at low (LR) and high (HR) resolutions (FOV=16cm; matrix = 200x200x16 (LR), 500x500x10 (HR); FA = 15; Slice Thickness = 3; TR/TE = 6.4/0.3 ms; total scan time = 35 seconds (LR), 51 seconds(HR)) All cones images were reconstructed with a temporal resolution of ~500ms.Reconstruction was performed as previously described using a multiscale low-rank (MSLR) reconstruction algorithm5 with a lambda value of 1e-6 and block widths of 32, 64, and 128 (LR) or 32, 64, 128, and 256 (HR). For comparison, a gridding and density compensation algorithm was used to create a fully sampled 3D image from the static data.
Results
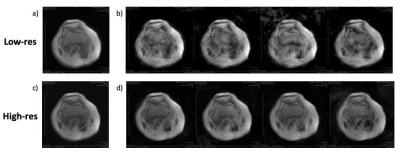
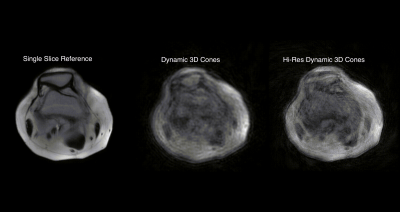
The first four time points from HR and LR static acquisitions are shown in figure 1 with fully sampled versions for comparison. Figure 2 shows an animation using 5 time points from HR and LR dynamic acquisitions as well as a reference 2D SSFSE acquisition. For simplicity, all figures display only one representative slice at various time points.Discussion
The high resolution static images have fewer artifacts than the low-resolution versions as seen in figure 1. This may be due to the fact that the MSLR recon takes advantage of data redundancies in the images and so may perform better when there is more data available. It is unclear if this translates to better dynamic (moving) images (figure 2). It is possible that the HR images do not have enough SNR for effective reconstructions. One possible solution to this is to acquire a larger FOV. This would allow us to acquire more data, hopefully leading to fewer artifacts, without increasing the resolution. This would also allow a larger range of motion without moving out of frame.While the dynamic MSLR reconstructions in figure 2 clearly have many artifacts, both the high resolution and low resolution reconstructions show motion of the same type and scale as the reference images. One advantage of joint imaging is the ability to obtain a high-resolution static image. This may allow for development of DL networks to remove some artifacts in the dynamic images. A 3D moving imageset like these could be used to develop statistical models to track the location and position of the bones in the joint during motion.
Another challenge with the current method is the offline reconstruction. Image reconstruction using the MSLR algorithm takes between 15 minutes and an hour depending on the size of the dataset. We are hopeful that we will be able to design a DL recon that can accelerate the reconstruction process and make it useful clinically.
Conclusion
We demonstrated the feasibility for 3D real-time imaging of the knee joint with a 3D golden-ratio re-ordered cones sequence with multiscale low-rank reconstruction. Additional optimization of the acquisition parameters and the use of deep learning to remove residual artifacts will further advance this approach to obtain clear, 3D, real-time MR images of a knee in motion.Acknowledgements
This work was supported by research funding from GE Healthcare.References
1. Malik, Khalid M., Rena Beckerly, and Farnad Imani. "Musculoskeletal disorders a universal source of pain and disability misunderstood and mismanaged: A critical analysis based on the US model of care." Anesthesiology and pain medicine 8.6 (2018)
2. Boutin, Robert D. et al. “Fast Musculoskeletal MRI: What the Radiologist Needs to Know” RSNA Educational Exhibit 23 October, 2019 Stanford, California
3. Clark, D., et al. "Mapping the contact area of the patellofemoral joint: the relationship between stability and joint congruence." The bone & joint journal 101.5 (2019): 552-558.
4. Laugharne E, Bali N, Purushothamdas S, Almallah F, Kundra R. Variability of Measurement of Patellofemoral Indices with Knee Flexion and Quadriceps Contraction: An MRI-Based Anatomical Study. Knee Surg Relat Res. 2016;28(4):297–301.
5. Ong, F., Zhu, X., Cheng, J. Y., Johnson, K. M., Larson, P. E., Vasanawala, S. S., & Lustig, M. (2020). Extreme MRI: Large‐scale volumetric dynamic imaging from continuous non‐gated acquisitions. Magnetic resonance in medicine, 84(4), 1763-1780.
Figures