1382
3D high-resolution Contrast-enhanced MR neurography of lumbosacral plexus with precise fat-suppression: A pilot image quality evaluation1Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China, 2Philips Healthcare, WuHan, China
Synopsis
The objective of this study was to investigate the values of precise fat-suppression for the robust visualization of 3D high-resolution contrast-enhanced MR neurography of lumbosacral plexus by inversion time (TI) scout technique. The precise TI of individuals could be calculated from several fast different TI experiments by measuring the fat signals recovery on the real and imaginary images. CNR (precise fat-suppression) (13.26±5.47) was about 425.4% higher than CNR (traditional TI) (2.39±0.55). Accurate fat suppression in MRN of lumbosacral plexus can help visual the branch of lumbosacral plexus nerves distinctly and improve the accuracy of diagnosis in diseases of lumbosacral plexus.
Introduction
The anatomical structure of the lumbosacral plexus is complex, which is easily affected by trauma, inflammation, tumors and other pathological changes. These diseases can even lead to lower limb dysfunction or lifelong disability. There is an urgent demand for precise diagnosis of the injured lumbosacral plexus and the degree of damage. In magnetic resonance neuroimaging, fat suppression plays an indelible role in neuroimaging, such as highlighting the nerve signal better, showing the shape and continuity of the nerve, improving the image quality related to fat (degradation、movement、chemical shift artifacts) [1,2]. Three-dimensional nerve-sheath signal increased with inked rest-tissue rapid acquisition of relaxation imaging (3D-SHINKEI), is widely used clinically for nerve imaging and has achieved good results[3]. The 3D-SHINKEI technology employed the Spectral Attenuated Inversion Recovery (SPAIR) for fat suppression. According to the manual from the vendor, the recovery time TI was preset based on experience. However, the precise TI for different patients could be different for optimized fat suppression. Therefore, the precise measurement of T1 values is very important for the MRN of the lumbosacral plexus[4]. However, the optimized TI changes as the parameters of the scanning protocol, and generally, the vendor doesn't provide the in-line calculation module. Hereby, a fast and easy method was demonstrated to get optimized TI value for lumbosacral plexus imaging by scanning several different TI values followed by an exponential fitting, which could improve the contrast effect of lumbosacral plexus neuroimaging.Methods
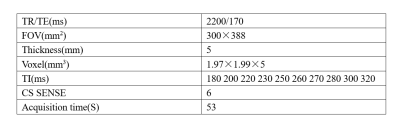
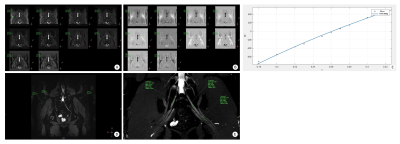
Patients: 32 patients were included in this study: 14 patients (group A) with preset TI,22 patients (group B) with accurately calculated TI values. All patients signed an informed consent form before the examination and were approved by the hospital ethics committee. All patients were scanned using a 3.0 T MR scanner (Ingenia CX, Philips Healthcare, the Netherlands) with a 32-element phased-array surface coil. After intravenous injection of Gd-DTPA (0.15mmol/kg), patients were scanned using the 3DNerveView sequence: the patients in group A have TI=220ms, and the patients in group B scan using the 3DNerveView (Philips Healthcare, 3D-SHINKEI based) sequence set different TI values, where TI=180 200 220 230 250 260 270 280 300 320 ms. Images were reconstructed on the scanner by the vendor-supplied software package (Compressed SENSE, Philips Healthcare). Measuring the fat signal value of the two groups of patients on the original graph, measuring the nerve signal value on the MIP graph, and calculating the nerve/fat signal ratio. The precise magnitude values of the fat signals were measured using the real and imaginary images, and an exponential fitting was used to obtain the TI values for the fat signals across zero, which provide the best fat suppression. Details of imaging protocols for 3DNerveView sequences were described in table 1. The subjective parameters of images were measured by an experienced radiologist. The signal intensity of fat and nerve was measured on the original graph and the MIP graph respectively and the signal intensity ratio of nerve to fat (NFR) was calculated for evaluation of fat suppression. Two senior radiologists analyze and research the images. The IBM SPSS22.0 software was used for statistical analysis, and the signal intensity ratio of nerve to fat between the two groups was compared by unpaired sample t-test. P<0.05 indicated a statistically significant difference.Results
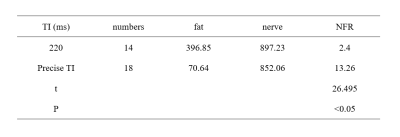
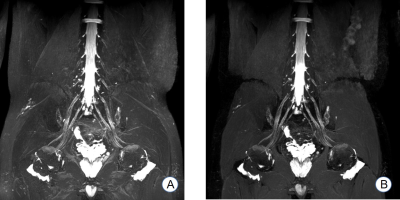
1. The proposed TI scout method could improve fat suppression in MRN dramatically. The calculated NFR (precise fat suppression) (13.26±5.47) was about 425.4% higher than that in the preset TI situation (220ms) (2.39±0.55). The difference between the two groups was statistically significant (t=26.495, P<0.05). (Table 2)2. The demonstration rates of nerve roots and trunks by the two methods were 100% (18/18,14/14); The demonstration rates of the nerve tracts and branches in precise fat-suppression sequence were 94.4% (17/18) and 83.3% (15/18), respectively. The demonstration rates of nerve tracts and branches in the traditional method were 92.9% (13/14) and 71.4% (10/14), respectively. There was no statistically significant difference between the two sequences in the display rate of nerve tracts and branches (P=1.00,0.67).
3. Two case reports (figure 1, figure 2):
Discussion
Injury of the lumbosacral plexus might lead to serious dysfunction and complications[1]. Early and accurate diagnosis is important for treatment and prognosis. The biggest challenge of MRI neuroimaging lies in the suppression of background signals including fat suppression[5]. However, precise fat suppression for lumbosacral plexus MRI has not been reported. Due to the individual differences in subjects and scanning protocols, the optimized TI values might be different for different patients. We demonstrated that optimized TI values could be obtained fast and easily with a TI scout technique, which showed the NFR is 425.4% higher than the traditional preset TI scheme. The proposed method could significantly improve the contrast noise ratio, fat suppression, and fat-related artifacts of MRN, which was important for highlighting the out-of-shape, continuity, and morphology of the lumbosacral plexus.Conclusion
A fast and easy TI scout-based strategy will be proposed to improve the fat suppression in 3D high-resolution contrast-enhanced lumbosacral plexus MRN, which showed promising clinical potentials.Acknowledgements
No acknowledgement found.References
[1] Filler A G, Maravilla K R, Tsuruda J S. MR neurography and muscle MR imaging for image diagnosis of disorders affecting the peripheral nerves and musculature[J]. Neurologic Clinics, 2004, 22(3):643-682.
[2] Zhang Y, Kong X, Zhao Q, et al. Enhanced MR neurography of the lumbosacral plexus with robust vascular suppression and improved delineation of its small branches[J]. European Journal of Radiology, 2020, 129:109128.
[3] Masami Y, Taro T, Kwee T C, et al. Rapid High Resolution MR Neurography with a Diffusion-weighted Pre-pulse[J]. Magnetic Resonance in Medical Sciences, 2013, 12(2):111-119.
[4] Andrew J, Taylor MD, Michael Salerno MD, et al. T1 Mapping: Basic Techniques and Clinical Applications[J]. Jacc Cardiovascular Imaging, 2016, 9(1):67-81.
[5] Freund W, Brinkmann A, Wagner F, et al. MR neurography with multiplanar reconstruction of 3D MRI datasets: an anatomical study and clinical applications. Neuroradiology, 2007, 49:335.
Figures