1381
Comparison of MR diffusion based tractography methods for reconstruction of the facial nerve in pre-operative vestibular schwannoma1Magnetic Resonance Physics, Guy’s & St. Thomas’ NHS Foundation Trust, London, United Kingdom, 2Department of Radiology, Guy’s & St. Thomas’ NHS Foundation Trust, London, United Kingdom, 3Clinical Scientific Computing, Guy’s & St. Thomas’ NHS Foundation Trust, London, United Kingdom, 4MRI, Guy’s and St. Thomas’ Hospitals & King’s College Hospital, London, United Kingdom, 5Neuroradiology, King’s College Hospital NHS Foundation Trust, London, United Kingdom
Synopsis
Four DWI tractography acquisitions are trialled across 13 pre-surgical patients with vestibular schwannomas: single shell EPI, ZOOMit, RESOLVE, & multi-shell RESOLVE, with an aim to reconstruct the path of the facial nerve. Data is analysed using MRtrix using multi-shell multi-tissue constrained spherical deconvolution (MSMT-CSD) and the probabilistic iFOD2 algorithm. The best reconstruction was achieved using a 30 direction multi-shell (b = 0, 300, 1000 s/mm2) RESOLVE acquisition scheme.
Introduction
Vestibular schwannomas (VS) are peripheral nerve sheath tumours arising from the vestibulocochlear nerve, which emerges from the brainstem and enters the structures of the inner ear via the internal auditory meatus (IAM). The facial nerve (FN), which runs alongside the vestibulocochlear nerve, is frequently displaced and flattened by VS. Preoperative identification of the course of the FN would be extremely useful to guide surgery and reduce the risk of FN injury. There is growing clinical interest in using diffusion imaging and diffusion tractography to identify and visualise the cranial nerves, however imaging remains challenging due to high susceptibility and geometrical distortions around the skull base.A recent literature review of diffusion imaging of cranial nerves found studies predominately used single-shot echo planar imaging (88%) and deterministic tractography methods (93%) [1]. More recent studies have demonstrated the improved accuracy of cranial nerve identification using RESOLVE [2] or multi-shell [3] acquisitions and probabilistic algorithms. In this study four tractography acquisitions were progressively trialled in pre-surgical patients with VS: single shell EPI, ZOOMit, RESOLVE, & multi-shell RESOLVE with an aim to find an optimal acquisition strategy for nerve bundle reconstruction.
Methods
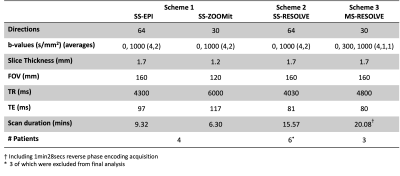
Data from 13 VS patients (54% male, mean age = 51 yrs and 38% right sided tumours) were scanned on a 3T Siemens Skyra system equipped with a 64 channel head coil, between July 2019 - November 2021. All procedures were in accordance with the ethical standards of the institutional research committee.The MR imaging protocol included an axial T1 weighted TSE (TR/TE, 600/12 ms; 2.20mins 0.4 ×0.4x2 mm), post-contrast-enhanced T2 CISS (TR/TE, 8.2/2.8ms; 4.57mins, 0.5× 0.5 × 0.5 mm) and one of three possible DTI acquisition schemes: single shell EPI & ZOOMit (n = 4), single shell RESOLVE (n = 6), and multi-shell RESOLVE (n = 3) see Table 1.
Post-processing steps (denoising, bias field correction, eddy correction) were performed using MRtrix [4]. Multi-shell multi-tissue constrained spherical deconvolution (MSMT-CSD) was performed, using two tissue types (CSF and WM) in single-shell data, and three (CSF, WM and GM) in multi-shell data, and the response function calculated using the dhollander algorithm. For comparison purposes, single shell data was also analysed using constrained spherical deconvolution (CSD) and the tournier algorithm. Whole brain tractography was performed using the probabilistic iFOD2 algorithm with the following parameters: number of streamlines = 500,000, step size = 1 mm, maximum angle = 45°, FA cutoff = 0.1. Streamlines were seeded entirely at random within the DWI image, no inclusion or exclusion ROIs were used and no seed points specified.
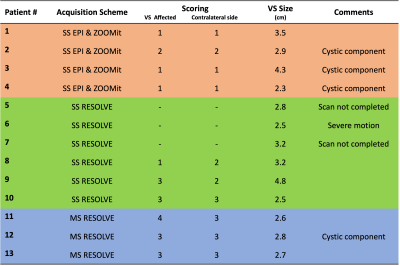
The results were scored as follows:
1. No reconstruction of a dominant nerve bundle
2. Partial reconstruction of a dominant nerve bundle
3. Full reconstruction of a dominant nerve bundle including tracking around the VS
4. Reconstruction of two distinct nerve bundles
Results
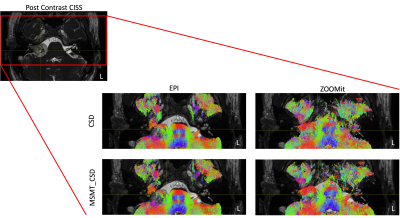
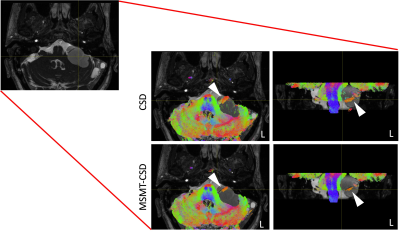
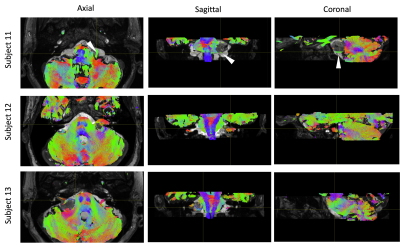
Of the 13 patients recruited, 2 were unable to complete the full imaging protocol due to reaction to contrast or claustrophobia, and 1 was excluded due to severe motion on the imaging. Table 2 shows the scoring of the nerve bundle reconstruction for each patient.Single-Shell: Partial reconstruction of a dominant nerve bundle was achieved in only one case using EPI and ZOOMit, see Figure 1. This was due to high levels of distortion and low SNR in EPI and ZOOMit DWI data respectively. RESOLVE yielded better results, with a nerve bundle through the IAM reconstructed in most cases and more successful tracking of nerve bundles around the tumour, see Figure 2, and an average score > 2. A comparison of using MSMT-CSD versus CSD in single shell data is shown in Figures 1 and 2.
Multi-shell: Multi-shell RESOLVE is the only method which produces an average score > 3, successfully tracking a dominant nerve bundle around the VS in all cases. This includes tumours which have a cystic component which have been shown to be more problematic for reconstruction [1].
Discussion
For single-shell acquisitions RESOLVE had reduced distortion in comparison to EPI and ZOOMit resulting in the best reconstruction of nerve bundles around a VS. Estimating the WM and CSF response functions in single-shell data, to correct for any free-water signal, reduced the spurious tracks within the tumour and surrounding space, however, did not result in improved scoring of reconstructions in these cases.Overall, the best reconstruction was achieved using a multi-shell RESOLVE acquisition scheme, which is consistent with recent literature findings [3]. In this study this was achieved despite using fewer diffusion directions (30) than is considered the gold standard (32-64), due to scan time constraints. The ~18 minute acquisition time of MS-RESOLVE could be halved using multiband techniques which already exist on clinical scanners, but were not available here [2].
The post-processing pipeline does not rely on manual seed placements or anatomically constrained ROI’s, resulting in reproducible results which are independent on the operator.
Conclusion
RESOLVE DWI tractography provides the best quality reconstruction of the vestibulocochlear and facial nerve bundle in the presence of VS. This is further improved by using a multi-shell acquisition (b = 0, 300, 1000 s/mm2). Based on these initial findings all subsequent patients recruited to the study will be scanned using the MS-RESOLVE acquisition scheme.Acknowledgements
The project is funded through the Guy’s and St. Thomas’ Charity.
Thanks to Amanda Hitchings (Clinical Nurse Specialist), Hayley Cheetham (Clinical Nurse Specialist), Adrian Green (Research trials nurse), John Spence (MRI Superintendent Radiographer), Ms Eleni Maratos, (Neurosurgeon), Mr Johnathan Shapey (Neurosurgeon), Mr Nick Thomas (Neurosurgeon), Mr Sinan Al-Barazi (Surgery), Mr Konstantinos Barkas (Neurosurgeon), Professor Dan Jiang (ENT surgeon) & Mr Rupert Oberholzer (ENT surgeon).
The authors would also like to acknowledge the radiography staff at Guy's & St Thomas' for their continued work and efforts supporting research within the department.
References
1] Shapey J, Vos SB, Vercauteren T, Bradford R, Saeed SR, Bisdas S and Ourselin S (2019) Clinical Applications for Diffusion MRI and Tractography of Cranial Nerves Within the PosteriorFossa: A Systematic Review. Front. Neurosci. 13:23. doi: 10.3389/fnins.2019.00023
[2] Yao Chia Shih et al., Trigeminal nerve tractography with accelerated simultaneous multislice readout-segmented echo planar diffusion tensor imaging. Proceedings of ISMRM 2020
[3] Castellaro M et al. Multishell Diffusion MRI–Based Tractography of the Facial Nerve in Vestibular Schwannoma. AJNR Am J Neuroradiol., 41 (2020), 1480–86
[4] J.-D. Tournier, R. E. Smith, D. Raffelt, R. Tabbara, T. Dhollander, M. Pietsch, D. Christiaens, B. Jeurissen, C.-H. Yeh, and A. Connelly. MRtrix3: A fast, flexible and open software framework for medical image processing and visualisation. NeuroImage, 202 (2019), pp. 116–37.
[5] Fung et al., DW-EPI distortion reduction using Multi-shot EPI (MUSE) and Reverse Polarity Gradient (RPG) in Head & Neck Region. Proceedings of ISMRM 2020
Figures