1320
Combined T2*-diffusion imaging of the fetal lungs in normal and preterm fetuses1Perinatal Health and Imaging, Kings College London, London, United Kingdom, 2Women and Children’s Health, Kings College London, London, United Kingdom, 3Department of Biomedical Engineering, Kings College London, London, United Kingdom, 4Centre for Medical Image Computing, UCL, London, United Kingdom
Synopsis
Advanced functional MRI techniques were applied to the fetal lungs to increase our understanding of in-utero lung development, imperative for accurate antenatal diagnosis to identify fetuses at highest risk of morbidity. Our preliminary results show that combined T2*-diffusion imaging is a feasible technique to analyse the developing lungs in utero. A reduction in both lung volumes and T2* values associated with fetuses that subsequently delivered preterm was identified - paving the way for future more detailed in depth studies.
BACKGROUND
While ultrasound is still the standard modality used for fetal imaging [1] eg to investigate pulmonary pathology, the role of antenatal MRI is growing [2]. Its advantages include the ability to robustly provide data until late gestation and is less dependent on maternal habitus as well as the availability of a range of additional contrasts allowing access to the microstructural and functional properties of tissue [3]. MRI has however not yet been as extensively validated in preterm birth and its consequences on the fetal lungs.3D volumetry of overall lung size has been studied using both ultrasound and MRI [4, 5], however these techniques are still limited as they do not provide information on the structural changes associated with some congenital conditions nor insight on how the lungs might function after birth. With the advent of advanced functional MRI parameters and development of post-processing techniques, proficient more detailed analysis is possible [6, 7]. The present study uses a combined T2*-Diffusion MRI acquisition of the fetal lungs to contribute to more in-depth antenatal lung characterisation including microstructure and oxygenation.METHODS
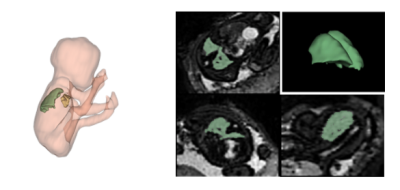
A group of pregnant women at gestational age(GA) between 20-32 weeks of gestation, classified as high or low risk for preterm delivery, were recruited. All women were scanned on a clinical 3T Philips Achieva MRI scanner using a 32-channel cardiac coil, with constant verbal interaction and life monitoring throughout the scan. A series of T2-weighted single shot fast spin echo sequences of the uterus was followed by a combined relaxometry-diffusion imaging [8] with a multi-echo single-shot echo planar imaging technique. The diffusion encodings were chosen with three diffusion gradient directions at b =[5,10,18,25,36,50,100,200, 400, 600, 800, 1200, 1600] s/mm2 [9].14 datasets, including 8 preterm(<32 weeks) and 6 control subjects( >37 weeks with no sign of major pregnancy complications) were post-processed following in-house-developed pipelines performing motion correction [10, 11], generating T2* and ADC maps using mono-exponential decay fitting. Regions-of-interest containing the lung tissue avoiding the vasculature were manually/automated segmented (Figure 1) on the resulting images to generate lung volumes as well as mean pulmonary T2* and ADC values. Furthermore, histograms were obtained from both the ADC and T2* values for each voxel within the lung mask.RESULTS
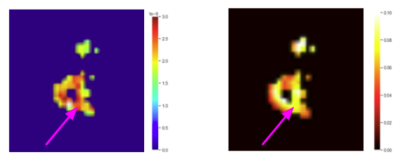
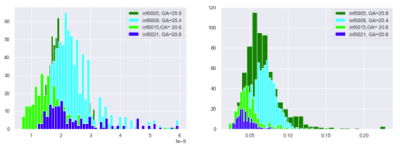
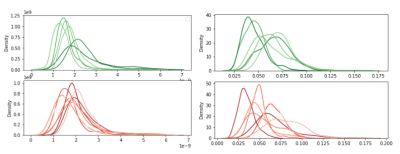
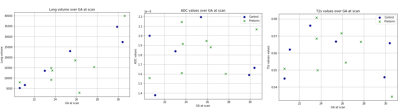
Initial results from the 8 datasets in the preterm cohort showed a reduction in pulmonary volume. The calculated T2* and ADC maps sampled from one exemplary preterm case showed increased ADC values close to the pulmonary vasculature(arrow) which appears to be reflected in its respective T2* map (Figure 2). Analysis of 4 models, including 2 controls and 2 preterm cases revealed a trend towards lower ADC and T2* values for the preterm cases at equivalent gestational ages and hints towards an increase of ADC values over GA (Figure 3). Visual histogram analysis confirmed this trend towards lower T2* values in the preterm cohort and a decreasing trend over GA can also be perceived (Figure 4). The impression of increasing ADC values over gestational age in the controls seems clearer when plotting all cases (Figure 5).Further quantitative analysis showed scattered mean pulmonary T2* and ADC values and showed no difference between fetuses delivered at term and preterm nor were found to clearly correlate with gestational age at present but this is ongoing work.DISCUSSION
Our findings of a reduction in pulmonary volume in fetuses delivered preterm are in keeping with previous work [12]. Although no clear difference between cohorts was observed with the calculated T2* and ADC maps at present, histogram-based analysis revealed trends towards significance. Analysis of paired spatially matched diffusion-T2* datasets such as these obtained for this study, could reveal additional molecular and functional tissue properties. Tissue displaying both low oxygen levels and low ADC values could thus be indicative of restricted diffusion, and might be correlated with impaired alveolarization. The T2* values analysed here were drawn from the combined T2*-diffusion datasets and when compared with their respective values obtained from the T2* images, a certain level of agreement was found between the two methods. These were observed to be lower in the preterm cohort compared to controls when individual T2* values were analysed which may reflect a reduction in metabolic activity of the tissue. Quantitatively this could not be observed here due to the nature of the files the lung masks were segmented on, and the amount of motion still present after reconstruction in certain files, potentially skewing the data given the small number of cases available for analysis. Visual analysis of the histograms corroborated the hypothesis of lower T2* values in the preterm cohort with a potential decrease over GA.CONCLUSIONS
This study provides original motion-corrected morphological and functional assessment of the antenatal fetal lung during normal compared to preterm development. These are preliminary results, but we can affirm that combined T2*-diffusion imaging is a feasible technique for analysis of the developing lungs in utero. Spatially-matched ADC and T2* values pave the way for future in-depth tissue analysis. Future work includes correlating the cases with abnormal T2* and diffusion values to establish whether those are the fetuses that develop adverse outcomes with the main aim of establishing individualised lung care and providing appropriate counselling and perinatal care.Acknowledgements
This work was supported by supported by the NIH Human Placenta Project grant 1U01HD087202-01 (Placenta Imaging Project (PIP)), Wellcome Trust Collaboration in Science grant [WT201526/Z/16/Z], a Sir Henry Wellcome Fellowship, a UKRI FL fellowship and by core funding from the Wellcome/EPSRC Centre for Medical Engineering [WT203148/Z/16/Z] and by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London and/or the NIHR Clinical Research Facility. Dr Lisa Story is funded by an NIHR Advanced Fellowship as a Clinical Lecturer for this project. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.References
1.Mon, R.A., et al., Diagnostic accuracy of imaging studies in congenital lung malformations. Archives of Disease in Childhood - Fetal and Neonatal Edition, 2019. 104(4): p. F372.
2. Reddy, U.M., et al., Prenatal imaging: ultrasonography and magnetic resonance imaging. Obstetrics and gynecology, 2008. 112(1): p. 145-157.
3.Balassy, C., et al., Diffusion-weighted MR imaging of the normal fetal lung. European radiology, 2008. 18: p. 700-6.
4.Kalache, K., et al., Three dimensional ultrasound fetal lung volume measurement: A systematic study comparing the multiplanar method with the rotational (VOCALTM) technique. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology, 2003. 21: p. 111-8.
5.Cannie, M.M., et al., Fetal body volume at MR imaging to quantify total fetal lung volume: normal ranges. Radiology, 2008. 247(1): p. 197-203.
6.Manganaro, L., et al., Diffusion-weighted MR imaging and apparent diffusion coefficient of the normal fetal lung: preliminary experience. Prenat Diagn, 2008. 28(8): p. 745-8.
7.Ho, A.E.P., et al., T2* Placental Magnetic Resonance Imaging in Preterm Preeclampsia: An Observational Cohort Study. Hypertension, 2020. 75(6): p. 1523-1531.
8.Hutter, J., et al., Integrated and efficient diffusion-relaxometry using ZEBRA. Scientific Reports, 2018. 8(1): p. 15138.
9.Slator, P.J., et al., Combined diffusion-relaxometry microstructure imaging: Current status and future prospects. Magn Reson Med, 2021. 86(6): p. 2987-3011.
10.Uus, A., et al. Deformable Slice-to-Volume Registration for Reconstruction of Quantitative T2* Placental and Fetal MRI. 2020. Cham: Springer International Publishing.
11.Slator, P.J., et al., Placenta microstructure and microcirculation imaging with diffusion MRI. Magnetic resonance in medicine, 2018. 80(2): p. 756-766.12.Story, L., et al., Foetal lung volumes in pregnant women who deliver very preterm: a pilot study. Pediatr Res, 2020. 87(6): p. 1066-1071.
12. Story, L., et al., Foetal lung volumes in pregnant women who deliver very preterm: a pilot study. Pediatr Res, 2020. 87(6): p. 1066-1071.
Figures