1317
Exploring coupling of venous blood and CSF fluid flow using flow sensitive Real-time phase-contrast MRI (PC-MRI) during forced breathing1University Medicine Göttingen, Göttingen, Germany, 2Max Planck Institute for Biophysical Chemistry, Göttingen, Germany
Synopsis
Venous system pathologies have increasingly been linked to disorders of CSF circulation whereas the exact coupling mechanisms still remain unknown. Using real-time phase-contrast MRI fluid dynamics of both systems were studied during normal and forced breathing in healthy subjects at spinal lumbar level L3. The aim was to provide experimental evidence that respiration couples CSF and venous flow. A correlation between CSF and venous flow could be observed during forced breathing. The findings point to a dynamic interplay between the fluid systems to regulate intracranial volume. Further insights will expand our understanding of the pathophysiology of different forms hydrocephalus.
Introduction
Venous system pathologies have increasingly been linked to clinically relevant disorders of CSF circulation1,2,3. However, the exact coupling mechanisms between these fluid systems still remain unknown. Investigating the driving forces of CSF and venous circulation and their correlation will improve our understanding of the pathophysiology of human diseases with CSF flow disturbances such as hydrocephalus and syringomyelia. The aim of the study is to provide experimental support that respiration couples CSF and venous fluid systems.Methods
Real-time phase-contrast MRI (PC-MRI) was performed on 16 healthy volunteers (age 28 ± 5 year) on a 3T Siemens scanner. During the measurement all volunteers followed a breathing protocol of 40 sec free breathing followed by 8 cycles of 2.5 s forced inspiration and 2.5 s forced expiration, closing with 10 sec of free breathing. PC-MRI was performed at spinal lumbar level three (L3) using the following acquisition parameters: TR: 5.68ms, TE: 4.62ms, in-plane resolution: 0.75 x 0.75 mm2, temporal resolution: 125ms per velocity map, VENC 60-100 cm/s. Regions of interest (ROI) were placed in the spinal subarachnoid space to quantify CSF flow. For corresponding venous flow, the epidural veins (EV) and the inferior vena cava (IVC) were chosen for ROI placements. Real-time flow-time curves were extracted from PC-MRI at each ROI using CaFuR software4,5. Coupling of CSF and venous flow during forced respiration was studied applying Pearson’s correlations.Results
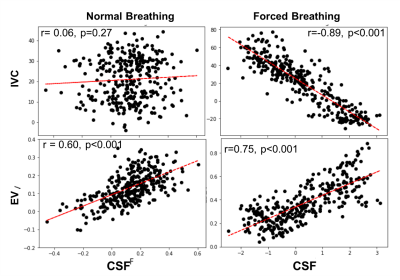
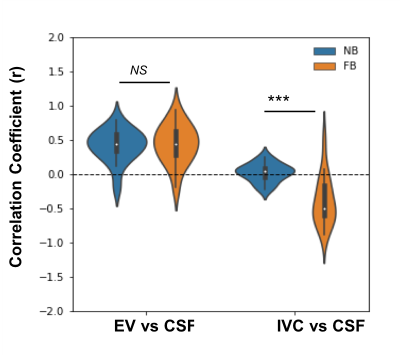
Respiration driven flow modulations were observed in both CSF and venous flow during forced breathing (Figure 1). Correlation between CSF and venous flow was found to be increased during forced respiration as compared to free breathing (Figure 2). Flow in IVC correlated negatively with CSF flow while flow in EV was positively correlated during forced breathing (Figure 3). The change in correlation coefficient due to forced respiration was significant for CSF vs IVC while no significance was found for CSF vs EV (Figure 3).Disscussion and Conclusion
During normal breathing the flow dynamics adhere to both respiration and cardiac pulsation thus a synchronization of CSF and venous flow is not detectable in the experimental data. However, with the onset of forced breathing, respiration becomes the dominant driving force of flow dynamics. In parallel a coupling of the two fluid systems can be observed. Negative correlation between CSF and IVC flow indicates an upward movement of CSF and simultaneous to that a downward venous flow during deep inhalation. During deep expiration the directionalities are reversed. The rapid respiration-dependent adjustments are assumed to be mediated by the transmission of adequate intrathoracic and intraabdominal pressure changes. A dynamic interplay between CSF and venous flow might play an important role regulating intracranial pressure and volumes according to the Monro Kellie doctrine and is in line with an increasingly popular holistic view on brain fluids6. The positive correlation between EV and CSF could be a result of a delayed response of the EV flow to the breathing protocol. It might also be due to a higher variability of the flow measurements due to the small vessel size and thus low level of flow. Further investigations are required to better understand the flow dynamics of smaller vessels like EV.Acknowledgements
No acknowledgement found.References
1. Elvsashagen, T. et al. Cerebral blood flow changes after a day of wake, sleep, and sleep deprivation. Neuroimage 186, 497-509 (2019).
2. Wilson, M.H. Monro-Kellie 2.0: The dynamic vascular and venous pathophysiological components of intracranial pressure. J Cereb Blood Flow Metab 36, 1338-50 (2016).
3. Dreha-Kulaczewski, S. et al. Identification of the Upward Movement of Human CSF In Vivo and its Relation to the Brain Venous System. J Neurosci 37, 2395-2402 (2017).
4. Joseph, A.A. et al. Real-time phase-contrast MRI of cardiovascular blood flow using undersampled radial fast low-angle shot and nonlinear inverse reconstruction. NMR Biomed 25, 917-24 (2012).
5. Chitiboi, T. et al. Context-based segmemtation and analysis of multi-cycle real-time cardiac MRI. IEEE International Symposium on Biomedical Imaging (2014) 943-946.
6. Nakada, T. & Kwee, I.L. Fluid Dynamics Inside the Brain Barrier: Current Concept of Interstitial Flow, Glymphatic Flow, and Cerebrospinal Fluid Circulation in the Brain. Neuroscientist 25, 155-166 (2019).
Figures