1305
Impact of breathing induced off-resonance on labeling efficiency in renal Arterial Spin Labeling1Division of MRI Research, department of Radiology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, United States
Synopsis
Renal Arterial Spin Labeling (ASL) is becoming more widely used as a non-invasive technique for measuring renal perfusion and hence renal function. Free-breathing acquisitions with retrospective motion-correction are commonly used as it facilitates workflow and is robust against uncooperative patients. However, PCASL, especially the balanced implementation in which the same net gradient is used for both label and control, has been shown to be sensitive to off-resonance leading to a loss of labeling efficiency. We propose here a pilot study measuring B0 shifts during free-breathing to simulate its impact on free-breathing renal PCASL perfusion imaging.
Introduction
Renal Arterial Spin Labeling (ASL) is becoming more widely used as a non-invasive technique for measuring renal perfusion and hence renal function. For that purpose, both pseudo-continuous ASL (PCASL) and Flow-Sensitive Alternating Inversion Recovery (FAIR) labeling schemes have been widely used and recommended as robust implementations. Free-breathing acquisitions with retrospective motion-correction are also commonly used as they facilitate workflow and are robust against uncooperative patients.However, PCASL, especially the balanced implementation in which the same net gradient is used for both label and control, has been shown to be sensitive to off-resonance leading to a loss of labeling efficiency (1,2). As it has been previously demonstrated that breathing can induce B0 fluctuations (3,4), especially close to the diaphragm, there is a concern that breathing-induced B0 shifts could severely impact PCASL labeling efficiency and therefore SNR and quantification accuracy. We propose here a pilot study measuring B0 shifts during free-breathing to simulate its impact on free-breathing renal PCASL perfusion imaging.Methods
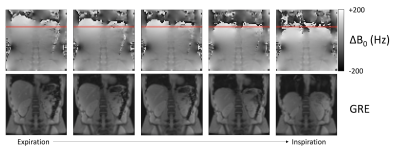
A single subject (female, 26y.o.) was scanned on a 3T scanner (GE Discovery MR750) using a 32-channel body array coil for reception. A dual-echo GRE B0 map was acquired during free-breathing using the following parameters: 34-cm FOV, 64x64 matrix, 10-mm slice thickness, coronal orientation, ΔTE=2.3ms. We also acquired in 3 minutes a free-breathing, single-slice unbalanced PCASL-SSFSE (Labeling/post-labeling = 1.5/1.5s, Coronal orientation, 128x128 matrix, 10-mm thickness, rBW=19.83kHz, TR/TE=7000/45ms) with optimized gradients (Gmax/Gav=3.5/0.5mT/m) to show the potential for free-breathing robust ASL.We then used data from the dynamic B0 map to simulate the effect of measured off-resonance at an 8-cm offset labeling plane as would be usually planned for a renal ASL scan. To do so, we positioned an ROI in the descending aorta where arterial blood would be labeled during the PCASL experiment. We numerically integrated Bloch equations and simulated the PCASL (500μs Hanning pulses played every 1ms) labeling fficiency in the following scenarios for a fixed spin velocity of 50cm/s and average B1 of 1.4μT:
- Balanced (same net gradient during label/control)
- Unbalanced (net gradient = 0 during the control acquisition)
We also compared the following gradient settings:
- Gmax=10mT/m, Gav=1mT/m, R=10
- Gmax=3.5mT/m, Gav=0.5mT/m, R=7
Results
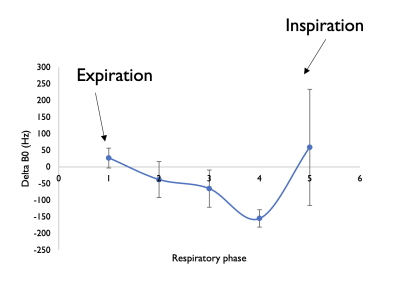
Over a typical respiratory cycle, we measured B0 fluctuations ranging from +27±30 Hz in full expiration to -155±30 Hz when reaching inspiration, as illustrated in Figures 1 and 2. However, the accuracy of the B0 map close to inspiration is questionable (phase 5). The interval of confidence (mean ± 1.96*SD) for phases 1 to 3 is estimated ranging from 85 to -174 Hz.When simulating labeling efficiency with those inputs, we calculated a theoretical labeling efficiency of 89.6% for the optimized unbalanced compared to 57% for balanced PCASL with standard gradient amplitudes. When increasing off-resonance to ±200 Hz, optimized unbalanced PCASL retained a high 85% efficiency while the balanced schemes efficiency lowered to 30 % efficiency.
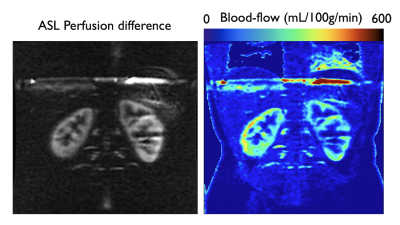
Figure 4 illustrates the typical high SNR renal perfusion data that can be acquired when using an unbalanced control with optimized gradient waveforms.
Discussion and Conclusions
We have measured in a human volunteer that breathing can induce B0 shifts of up to +/- 200 Hz at the level of the diaphragm, which was shown by simulation to cause up to 70% loss of labeling efficiency with balanced PCASL mainly due to inefficiency in the control condition. This can have a highly detrimental effect on image quality by lowering the perfusion SNR but also causing significant inaccuracies. The use of an unbalanced scheme is very robust against off-resonance as previously reported in the brain (1) and kidneys (2,5), and especially in the range of off-resonance that can be encountered during a typical breathing cycle. These theoretical results should of course be confirmed experimentally in a bigger cohort.To conclude, although preliminary, this work shows that while free-breathing causes significant B0 fluctuations at the labeling plane, the use of an unbalanced labeling scheme with optimized gradient peak and average amplitudes leads to very minimal loss of labeling efficiency compared to balanced PCASL and/or “standard” gradient settings. Altogether, this shows that free-breathing PCASL is robust against off-resonance given the above-mentioned considerations.Acknowledgements
No acknowledgement found.References
1. Zhao L, Vidorreta M, Soman S, Detre JA, Alsop DC. Improving the robustness of pseudo-continuous arterial spin labeling to off-resonance and pulsatile flow velocity. Magn. Reson. Med. 2017;78:1342–1351 doi: 10.1002/mrm.26513.
2. Echeverria‐Chasco R, Vidorreta M, Aramendía‐Vidaurreta V, et al. Optimization of pseudo‐continuous arterial spin labeling for renal perfusion imaging. Magn. Reson. Med. 2021;85:1507–1521 doi: 10.1002/mrm.28531.
3. Jahanian H, Noll DC, Hernandez-Garcia L. B0 field inhomogeneity considerations in pseudo-continuous arterial spin labeling (pCASL): effects on tagging efficiency and correction strategy. NMR Biomed. 2011;24:1202–1209 doi: 10.1002/nbm.1675.
4. Verma T, Cohen-Adad J. Effect of respiration on the B0 field in the human spinal cord at 3T. Magn Reson Med 2014;72:1629–36 doi: 10.1002/mrm.25075.
5. Zhou L, Wang Y, Madhuranthakam AJ. Improving the robustness of pseudo-continuous arterial spin labeling for renal perfusion imaging. In: Vol. 29. Virtual; 2021. p. 2539.
Figures