1218
Improved visualization of intracranial peripheral arteries with multiple 2D slice ASL-MRA and super-resolution1Wellcome Centre for Integrative Neuroimaging, FMRIB, Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, United Kingdom, 2Department of Radiology, NorthShore University HealthSystem, Evanston, IL, United States, 3Pritzker School of Medicine, University of Chicago, Chicago, IL, United States
Synopsis
In recent years, magnetic resonance angiography (MRA) using arterial spin labeling (ASL) technique has been developed aiming to be a non-invasive potential alternative to X-ray angiography. When blood flow is slow (e.g. in elderly patients, especially with steno-occlusive diseases), however, ASL-MRA suffers from poor vessel visualization, which hinders its clinical utility in those patients. In this study, instead of using a 3D volume acquisition commonly used in brain MRI, we propose to separately scan multiple 2D slices to reduce the saturation of arterial blood signal and improve the visualization of small peripheral arteries, in combination with a super-resolution reconstruction.
Introduction
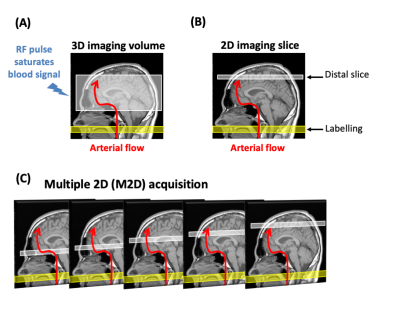
Arterial Spin Labeling (ASL) utilizes arterial blood itself as an endogenous tracer by magnetically “labeling” it, thereby making dynamic magnetic resonance angiography (MRA) using ASL a non-invasive potential alternative to X-ray angiography. Similar to X-ray angiography, vessel-selective ASL enables the exclusive visualization of a targeted arterial tree. Non-invasive examination is beneficial for patients with known or suspected cerebrovascular diseases, especially pediatric patients. Although scan time for ASL-MRA is relatively long, recent research shows that the use of undersampled golden-angle radial trajectory in conjunction with compressed-sensing is suitable for ASL-MRA because of its high sparsity in the image domain after subtraction1, which makes ASL-MRA feasible in clinical examinations.When blood flow is slow, however, ASL-MRA suffers from poor vessel visualization, which is common in elderly patients, especially with steno-occlusive diseases. This problem hinders its utility in those patients if being considered as an alternative to X-ray angiography. In brain MRA, a 3D ‘volume’ acquisition is typically used to cover the large volume of the brain with high spatial resolution. However, repeated application of RF pulses to the whole brain during 3D imaging markedly saturates arterial blood signal as it flows further distally into the brain (Figure-1a). In this proof of concept study, we propose to separately scan multiple 2D (M2D) slices (Figure-1b and c), instead of a 3D volume, to reduce the saturation of arterial blood signal and improve the visualization of small peripheral arteries. However, obtaining thin 2D slices to achieve a typical spatial resolution of 0.5-1.5mm required for brain MRA is hampered by limitations of the MRI hardware and a low signal-to-noise ratio. In this work, a super-resolution reconstruction was tested to solve this problem.
Methods
Our M2D ASL-MRA consists of pseudo-continuous ASL (PCASL) labeling and a 2D FLASH readout, in which only a single slice is excited after each labeling period (Figure-1c). Immediately after a 500ms PCASL labeling module, six dynamic phases were acquired by a Look-Locker readout with an interval of 198ms. Intracranial arteries of two healthy volunteers (1 Female, 30 and 44 y/o) were scanned with imaging parameters as follow: FOV = 200 x 200mm, Matrix = 176 x 176, slice thickness = 3mm with overlap of 50% (1.5mm), 60 slices, in-plane GRAPPA factor = 3, flip angle = 26°. Scan time was 6:59. For comparison, a conventional 3D FLASH sequence was also acquired with the same imaging parameters (except 1.5mm slice thickness and flip angle = 10°), and its scan time was 6:33. All scans were performed on a Siemens 3T Prisma under a technical development protocol agreed by local ethics and institutional committees.
Super-resolution reconstruction was applied in the slice direction of the acquired M2D images using the iterative back-projection algorithm of Irani and Peleg2.
In addition to the maximum intensity projection (MIP) in the transverse, sagittal and coronal directions, MIPs were produced across the temporal dimension (temporal-MIP).
Results
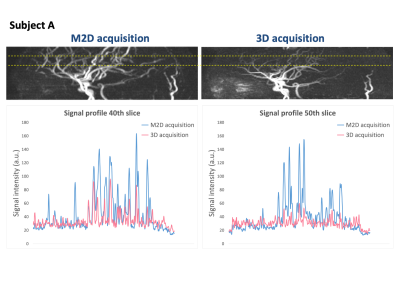
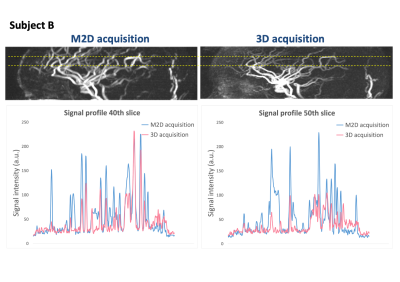
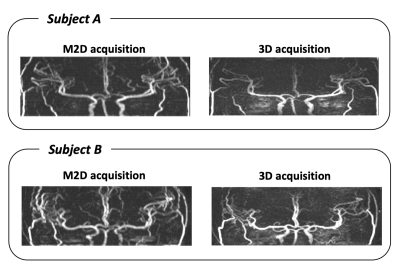
Figure-2 shows a comparison of the sagittal MIP images acquired with M2D and 3D acquisitions. The visualization of peripheral arteries shown in later phases (indicated by yellow arrows) is notably stronger in the M2D acquisition. The same result is also confirmed by the sagittal and coronal temporal-MIPs and signal profiles along two lines on the sagittal temporal-MIP (at the levels of 40th and 50th slices; indicated with yellow dashed lines) as shown in Figures 3, 4 and 5. M2D could depict more vessels with high signal intensity in distal area and difference is more prominent in the higher slice location. In general, however, vessel visualization by M2D is blurrier than 3D; where the vessels are visualized (relatively proximal area), 3D acquisition provides sharper and smoother depiction.Discussion and conclusion
M2D acquisition is commonly used for time-of-flight (TOF) MRA outside the brain, where M2D acquisition helps to retain the inflow blood signal even while providing large head-foot coverage. In the brain, however, the use of M2D TOF-based acquisition is hindered by the highly tortuous vessel anatomy; the venous saturation slab positioned above the imaging slice could suppress arterial blood signal as it flows inferiorly in tortuous arterial segments. In contrast, ASL does not require a superior saturation slab to suppress the venous signal, thereby making the use of M2D feasible.There are two important limitations of the proposed approach that should be addressed in future work. First, due to scan time considerations, the slice overlap in the slice direction used with the super-resolution reconstruction was only 50% in this study, which limited the achievable spatial resolution and image quality. In future work, measures to reduce scan time and/or the use of more advanced super-resolution approaches will be attempted. Second, in M2D acquisition, the influence of motion appears as slice misalignment, which could be rather obvious (as compared to 3D acquisition, in which subject motion will corrupt the entire 3D imaging volume). In future work, a slice-to-volume registration will be implemented to address such inter-slice misalignments, which could make M2D acquisition especially beneficial in the imaging of restless patients who move frequently during the exam.
In this proof of concept study, we have shown that M2D-ASL was able to visualize more peripheral arteries with higher signal intensity than the conventional 3D acquisition.
Acknowledgements
This project was supported by the Royal Academy of Engineering under the Research Fellowship scheme (RF\201920\19\236). The Wellcome Centre for Integrative Neuroimaging is supported by core funding from the Wellcome Trust (203139/Z/16/Z). PJ thanks the Dunhill Medical Trust and the Oxford NIHR Biomedical Research Centre for support. TO was supported by a Sir Henry Dale Fellowship jointly funded by the Wellcome Trust and the Royal Society (Grant Number 220204/Z/20/Z).References
1. Schauman, S. S., Chiew, M. & Okell, T. W. Highly accelerated vessel-selective arterial spin labeling angiography using sparsity and smoothness constraints. Magn. Reson. Med. 83, 892–905 (2020).
2. Koktzoglou, I. & Edelman, R. R. Super-resolution intracranial quiescent interval slice-selective magnetic resonance angiography. Magn. Reson. Med. 79, 683–691 (2018).
Figures