1177
Intra-Visit and Inter-Visit Repeatability of 129Xe Multiple-Breath Washout MRI in Children with Stable Cystic Fibrosis Lung Disease
Faiyza Shoaib Alam1,2, Brandon Zanette2, Sharon Braganza2, Daniel Li2, Felix Ratjen2,3, and Giles Santyr1,2
1Medical Biophysics, University of Toronto, Toronto, ON, Canada, 2Translational Medicine, Hospital for Sick Children, Toronto, ON, Canada, 3Division of Respirology, Hospital for Sick Children, Toronto, ON, Canada
1Medical Biophysics, University of Toronto, Toronto, ON, Canada, 2Translational Medicine, Hospital for Sick Children, Toronto, ON, Canada, 3Division of Respirology, Hospital for Sick Children, Toronto, ON, Canada
Synopsis
Hyperpolarized 129Xe MRI (Xe-MRI) yielding VDP has shown advantages over conventional PFT’s for assessing paediatric CF lung disease but is only a static “snapshot” of a dynamic process. Xe-MRI can be conducted in a MBW fashion to yield temporal/spatial heterogeneity of the gas during respiration, resulting in regional maps of fractional ventilation (r), a measure of percent gas clearance per breath. This work assessed the within-visit and inter-visit repeatability of MBW Xe-MRI between baseline and one-month follow-up in paediatric subjects with stable CF and found strong intra- and inter-visit repeatability. Significant correlations between MBW Xe-MRI and LCI were also found.
Introduction
As life expectancy of cystic fibrosis (CF) patients improves, the utility of conventional pulmonary function tests (PFTs), such as spirometry, to observe early lung function changes is limited, giving healthy results in paediatric CF patients1. The lung clearance index (LCI), a research-based method2 derived from the multiple breath washout (MBW) test, is more sensitive to paediatric CF than spirometry3. LCI is limited to whole-lung averages of the temporal heterogeneity of washout4. Hyperpolarized 129Xe MRI (Xe-MRI) yielding ventilation defect percent (VDP) visualizes the spatial distribution of lung ventilation. It significantly correlates with LCI5, is reproducible over a few weeks in stable CF4,6, and longitudinal imaging detects functional changes not reflected in PFTs4,6. However, it is a static “snapshot” of an inherently dynamic process.Xe-MRI can be conducted in a MBW fashion to yield temporal/spatial heterogeneity of the gas during respiration, resulting in regional maps of fractional ventilation (r), a measure of percent gas clearance per breath4,7,8,9. Unlike VDP, this method provides insight into temporal dynamics of gas mixing, similar to LCI, while providing additional spatial information that is potentially more sensitive to disease progression. Before MBW XeMRI is used to assess treatment response in paediatric CF studies, the within-visit and inter-visit repeatability of the method in stable CF must be established. In this work, the within-visit and inter-visit repeatability of MBW Xe-MRI between baseline and one-month follow-up in paediatric subjects with stable CF is shown.
Methods
This study was approved by the SickKids research ethics board. Written consent was obtained from parents/guardians. 23 subjects were recruited (5 healthy, 18 stable CF, median age 15 [range=11-18]), with 2 visits each (baseline, one-month). For 9 subjects, intra-visit repeatability was assessed with repeat scans (6 CF, 3 healthy). Each visit contained spirometry/plethysmography for forced expiratory volume in one second (FEV1, TLC), N2 MBW for lung clearance index (LCI), and HP 129Xe MBW MRI for fractional ventilation (r) and coefficient of variation (CoV) maps (defined as the standard deviation over mean of r in one pixel compared to neighbouring pixels).129Xe was polarized using a commercial polarizer (Polarean 9820) and dosed to 10% of TLC based on height/sex10. The bag was topped with buffer (N2) for a total volume of 1/6th TLC and inhaled from FRC. HP 129Xe MBW imaging was performed as described by Couch et al4, with data analysis performed using the variable T1 method4.
For statistical analysis, the Pearson correlation (R), coefficient of variation (CV%), coefficient of reproducibility (CR), and inter-class coefficient (ICC) were calculated for LCI, FEV1, and r and CoV map means. Health (rH, CoVH, LCIH and FEV1H) and CF (rCF, CoVCF, LCICF and FEV1CF) were separated. The correlation of r/CoV with PFT’s was also tested.
Results
R, CV%, CR, and ICC are listed in Table 1.Intra-visit ICC values for rH,CF and CoVCF were significant, with rH excellent (0.930) and others moderate (rCF 0.766, CoVCF 0.723, CoVH 0.741). As expected, intra-visit CR and CV% was smaller than inter-visit.
Inter-visit ICC for rH was excellent (0.949) and higher than other healthy metrics (CoVH [0.720], FEV1H [0.637], LCIH [-0.699], latter two not significant). R was excellent for rH (0.921) only. In CF, R was excellent/significant for all metrics. Surprisingly, repeatability was stronger in CF compared to health for all metrics except r.
Figure 1 shows the strongest correlation, CoVCF with LCICF (R=0.55). Additionally, CoV distinguished health from disease at 5% significance while r did not.
Figure 2 contains representative r and CoV maps.
Discussion
Overall, intra- and inter-visit repeatability for MBW XeMRI (ie. rH,CF and CoVH,CF) was high. The significance of intra-visit repeatability for CoVH is likely affected by low sample size, but ICC trends in the correct direction and will likely improve with more subjects.The higher inter-visit repeatability in CF versus health for CoV, LCI and FEV1 was unexpected, but may result from the small sample size of healthy controls. Additionally, ventilation defects in stable CF may serve as anchors to improve repeatability, with such anchors non-existent in healthy subjects. For r, the ventilation manoeuvre is potentially easier for healthy subjects, making rH more repeatable than rCF.
The ability of CoV to distinguish health from disease and correlate with LCI in CF is interesting, especially with r more repeatable than CoV (intra/inter-visit). CoV was previously shown to be useful for VDP mapping in asthma11 and describes the inherent heterogeneity of r, while r describes lung turnover efficiency. This may point to the importance of spatial heterogeneity of r in CF compared to the average value of r, a finding consistent with previous work9.
With repeatability established, MBW XeMRI may provide a novel approach for following pediatric CF lung disease progression/treatment response. One limitation is the inability to probe more diseased lung areas in CF subjects due to gas obstruction. Future research would benefit from more healthy controls to bolster assessment of baseline reproducibility without disease and explore longer wash-in/out dynamics using 19F-PFP gas12.
Conclusion
MBW XeMRI has strong inter-visit repeatability for both rH.CF and CoVH,CF. The intra-visit repeatability is also high for r in health and CF, and in CoV for CF. CoV also distinguished health from disease and correlates significantly with LCI.Acknowledgements
Funding and studentship was provided by the Canadian Institute for Health Research (CIHR) and the Cystic Fibrosis Foundation (CFF). Thanks to Jacky Au, Yonni Friedlander, Samal Munidasa, Leslie Burns, Tammy Rayner, and Ruth Weiss for assistance with imaging experiments.References
1. Marshall, B, et al. (2020). Cystic Fibrosis Foundation Patient Registry 2019 Annual Data Report [Ebook] (p. 43). Bethesda: Cystic Fibrosis Foundation. Retrieved from https://cff.org/Research/Researcher-Resources/Patient-Registry/2019-Patient-Registry-Annual-Data-Report.pdf2. Perrem, L., Rayment, J., & Ratjen, F. (2018). The lung clearance index as a monitoring tool in cystic fibrosis. Current Opinion In Pulmonary Medicine, 24(6), 579-585. Doi: 10.1097/mcp.0000000000000515
3. Stanojevic, S., Davis, S., Retsch-Bogart, G., Webster, H., Davis, M., & Johnson, R. et al. (2017). Progression of Lung Disease in Preschool Patients with Cystic Fibrosis. American Journal Of Respiratory And Critical Care Medicine, 195(9), 1216-1225. Doi: 10.1164/rccm.201610-2158oc
4. Couch, M., Morgado, F., Kanhere, N., Kowalik, K., Rayment, J., Ratjen, F., & Santyr, G. (2019). Assessing the feasibility of hyperpolarized 129 Xe multiple‐breath washout MRI in pediatric cystic fibrosis. Magnetic Resonance In Medicine, 84(1), 304-311. Doi: 10.1002/mrm.28099
5. Kanhere, N., Couch, M., Kowalik, K., Zanette, B., Rayment, J., & Manson, D. et al. (2017). Correlation of Lung Clearance Index with Hyperpolarized 129Xe Magnetic Resonance Imaging in Pediatric Subjects with Cystic Fibrosis. American Journal Of Respiratory And Critical Care Medicine, 196(8), 1073-1075. Doi: 10.1164/rccm.201611-2228le
6. Smith, L., Horsley, A., Bray, J., Hughes, P., Biancardi, A., & Norquay, G. et al. (2020). The assessment of short- and long-term changes in lung function in cystic fibrosis using 129Xe MRI. European Respiratory Journal, 56(6), 2000441. Doi: 10.1183/13993003.00441-2020
7. Horn, FC., Deppe, MH., Marshall, H., Parra-Robles, J., Wild, JM. Quantification of regional fractional ventilation in human subjects by measurement of hyperpolarized 3He washout with 2D and 3D MRI. J Appl Physiol. 2014;116;129-139.
8. Horn, FC., Rao, M., Stewart, NJ., Wild, JM. Multiple breath washout of hyperpolarized 129Xe and 3He in human lungs with three-dimensional balanced steady-state free-precession imaging. Magn Reson Med. 2017;77;2288-2295.
9. Horn, FC., Marshall, H., Siddiqui, S., Horsley, S., Smith, L., & Aldag, I. et al. (2015). Ventilation heterogeneity in obstructive airways disease – comparing multi-breath washout-imaging with global lung measurements. [Abstract]. Proc Intl Soc Mag Reson Med. 2015;23.
10. Thomen, R., Walkup, L., Roach, D., Cleveland, Z., Clancy, J., & Woods, J. (2017). Hyperpolarized 129Xe for investigation of mild cystic fibrosis lung disease in pediatric patients. Journal Of Cystic Fibrosis, 16(2), 275-282. doi: 10.1016/j.jcf.2016.07.008
11. Safavi, S., Munidasa, S., Zanette, B., Dai, R., Stirrat, E., & Li, D. et al. (2021). Evaluating post-bronchodilator response in well-controlled paediatric severe asthma using hyperpolarised 129Xe-MRI: A pilot study. Respiratory Medicine, 180, 106368. doi: 10.1016/j.rmed.2021.106368
12. McCallister, A., Chung, S., Antonacci, M., Powell, M., Ceppe, A., & Donaldson, S. et al. (2020). Comparison of single breath hyperpolarized 129 Xe MRI with dynamic 19 F MRI in cystic fibrosis lung disease. Magnetic Resonance In Medicine, 85(2), 1028-1038. doi: 10.1002/mrm.28457
Figures
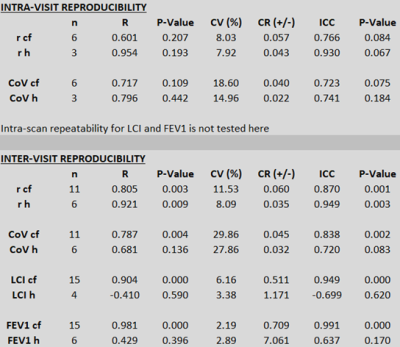
Table 1: Of 23 subjects over two visits, 6 CF and 3 healthy participants were able to undergo same-day scan repeats. For inter-visit reproducibility, 11 CF subjects had viable first and second visit scans, with 6 for healthy subjects. Only 4 healthy subjects had viable inter-visit LCI data. Significance in health may be affected by low sample size. The ICC values for r and CoV in both health and CF show high repeatability, with R showing good correlation for all metrics except CoVH.
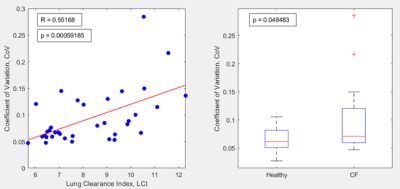
Figure 1: (Left) Correlation between CoV and LCI in CF subjects. R and p value from the Pearson correlation are directly on the figure. (Right) Boxplots for CoV values in healthy and CF. A two-sample t-test for equal means was used to distinguish between boxplots. The p value from the t-test is listed in the top left and is significant within 5%. Healthy distribution does not have outliers and is more well-behaved than CF, which exhibits a bigger skew (outliers in red crosses). The CF distribution also has a higher mean (i.e. more heterogeneity) than in healthy (CF: 0.0936, healthy: 0.0647).
Figure 2: r (top row) and CoV (bottom row) maps for A: a representative healthy subject (subject 16) and B: a representative CF subject (subject 20). Visit and scan repeat number are listed on the image, with intra-visit repeat occurring on visit 2 for the healthy subject and visit 1 for the CF subject. White arrows point to an example of a consistency between repeat scans/visits in each of the r/CoV maps. Regions that are completely black (ex. blue arrow) are artificially masked and do not represent ventilation defects but are instead artifacts of the processing pipeline4.
DOI: https://doi.org/10.58530/2022/1177