1168
Hyperpolarized 129Xe MRI and spectroscopy in healthy control subjects reveals age-related changes in measurements of pulmonary gas exchange1Radiology, Duke University, Durham, NC, United States, 2Medicine, Duke University, Durham, NC, United States, 3Biomedical Engineering, Duke University, Durham, NC, United States, 4Mechanical Engineering, Duke University, Durham, NC, United States, 5Physics, Duke University, Durham, NC, United States, 6Medical Physics, Duke University, Durham, NC, United States
Synopsis
Age-related changes in 129Xe gas exchange MRI and spectroscopy are not well understood. We assessed a suite of common 129Xe-derived measures of gas exchange function in a population of healthy control subjects age 19-87. Increased age was associated with reduced red blood cell (RBC) to barrier ratio and with greater levels of ventilation defects and RBC transfer defects. These effects must be accounted for when evaluating 129Xe-derived metrics as markers of disease in individual patients. Notably, high barrier uptake remained largely minimal across age groups, and does not appear to be a feature of healthy aging.
INTRODUCTION
A range of metrics derived from hyperpolarized 129Xe gas exchange MRI and spectroscopy have been proposed as potential markers of disease progression and therapy response in diverse pulmonary diseases ranging from asthma and COPD to interstitial lung disease and radiation-induced lung injury. However, the way in which these 129Xe measurements change in the context of healthy aging is poorly understood. Characterizing these changes is necessary for differentiating disease-driven abnormalities from expected consequences of aging. Here, we examine a range of commonly acquired 129Xe measurements of gas exchange in the context of a healthy aging, including the red blood cell (RBC) to barrier ratio (RBC:Barrier) derived from 129Xe spectroscopy, and four imaging-based measurements: the ventilation defect percent (VDP), barrier defect percent (BDP), high barrier percent (HBP), and the RBC defect percent (RDP).METHODS
PopulationSubjects (N=37, 11F/26M, age 45.3±18.5yrs, min 19 max 87) with no history of pulmonary disease and less than 5 pack-years of smoking with no tobacco use within the last 5 years underwent hyperpolarized 129Xe MRI and spectroscopy.
Acquisition
Signals from gas phase (airspaces) and dissolved phase (interstitial barrier tissue uptake and red blood cell [RBC] transfer) were acquired during a single breath-hold1. This process generated 3D images of the gas, barrier, and RBC components with a nominal isotropic resolution of 6.3mm. The gas-phase 129Xe images were rendered into quantitative binning maps with thresholds derived from a healthy reference cohort, as described previously.2 The ratio of RBC to barrier signal (RBC:Barrier) was obtained from 129Xe spectroscopy.3
Statistical Analysis
On spectroscopy, we evaluated the correlation between RBC:Barrier and age using the Pearson correlation. We further modeled RBC:Barrier as a function of both age and sex using a linear regression model with fixed effects. To compare image-based binning metrics, subjects were stratified into 3 age groups: <30yrs, 30-49yrs, and 50+ yrs. We then compared VDP, BDP, HBP, and RDP across age categories using the non-parametric Wilcoxon rank-sum test with a Holm-Bonferroni correction for multiple comparisons.
RESULTS
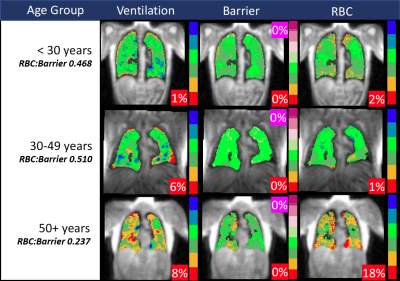
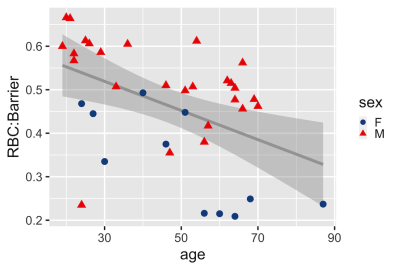
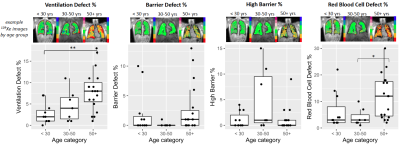
Eleven subjects (29.7%) were in the < 30yr category; 7 subjects (18.9%) were 30-49yrs; and 19 subjects (51.3%) were 50+ yrs. Images and RBC:Barrier values from example subjects in each age group are shown in Figure 1.On 129Xe spectroscopy, RBC:Barrier was negatively correlated with age as a continuous variable (r = -0.47, p = 0.003), as shown in Figure 2. In the multivariate linear fixed effects model with RBC:Barrier as the outcome, both age and sex were significant predictors. Each additional 10 years of age was associated with a 0.02 decrease in RBC:Barrier (p=0.002). Male sex vs. female was associated with an RBC:Barrier increase of 0.17 (p<0.001). For the imaging analysis, VDP was significantly higher in the 50+ yr group vs. <30 (median [1Q-3Q] of 8.0 [5.5-10]% vs. 2.0% [1.0%-3.5%], p=0.004), as shown in Figure 3. RDP was significantly higher in the 50+ yr group (9.5 [4.8-18.0]%) vs. the 30-49yr group (3.0 [2.0 – 5.0]%, p=0.035) and on the cusp of significance vs. the <30 group (2.0 [2.0 – 8.0]%, p = 0.055). There were no significant differences in barrier measurements (BDP and HBP) across age groups, with median values of 0-1% across all age groups for both metrics.
DISCUSSION
Understanding the effects of healthy aging on 129Xe gas exchange MRI and spectroscopy is essential for differentiating disease-driven processes from expected consequences of aging, and for establishing age-based reference values. The models in this study suggest that both age and sex are significant predictors of the RBC:Barrier value derived from 129Xe spectroscopy.These results further suggest that elevated ventilation defects and RBC transfer defects may be a common feature of older patients with no diagnosed pulmonary abnormalities. Measurements of ventilation defects exhibited a general upward trend with age, while RBC defects were predominantly present in only the 50+ group.
In contrast, interstitial barrier signal appeared to be relatively stable and preserved across the age categories, suggesting that barrier abnormalities may be a consistent marker of an underlying disease process. Interestingly, there were several outliers in the 50+ group with elevated barrier defect, possibly the result of undiagnosed emphysema. The significance of the handful of subjects with high barrier in the 30-49yr group is unclear, especially considering the near-uniform absence of high barrier in the 50+ year population.
Increasing the number of subjects in our study, especially in the 30-49yr population, will enable a comprehensive analysis of these patterns.
CONCLUSION
Healthy control subjects with no history of pulmonary disease exhibit significant age-related variations on 129Xe gas exchange MRI and spectroscopy, and these effects must be accounted for when assessing 129Xe-derived metrics as markers of disease in individual patients. Notably, high barrier uptake remained minimal across age groups, and does not appear to be a feature of healthy aging.Acknowledgements
Supported by NIH/NHLBI R01HL105643References
1. Niedbalski PJ, Hall CS, Castro M, et al. Protocols for multi‐site trials using hyperpolarized 129Xe MRI for imaging of ventilation, alveolar‐airspace size, and gas exchange: A position paper from the 129Xe MRI clinical trials consortium. Magn Reson Med 2021;
2. Wang Z, Robertson SH, Wang J, et al. Quantitative analysis of hyperpolarized 129Xe gas transfer MRI. Med Phys 2017;44(6):2415–2428.
3. Bier EA, Robertson SH, Schrank GM, et al. A protocol for quantifying cardiogenic oscillations in dynamic 129Xe gas exchange spectroscopy: The effects of idiopathic pulmonary fibrosis. NMR Biomed 2019;32(1):e4029.
Figures