1086
New Endo Coil and Novel Methods for Improving mpMR-TRUS Guided Fusion Prostate Biopsies with Hyperpolarized C-13 Pyruvate Molecular Imaging1Bioengineering, University of California, San Francisco, CA, United States, 2School of Medicine, University of California, San Francisco, CA, United States, 3Radiology and Biomedical Imaging, University of California, San Francisco, CA, United States
Synopsis
A new 13C/1H endorectal coil was designed, 3D printed, and manufactured with optimal dimensions to improve the comfort and tolerability for patients and provide higher SNR over the original endorectal coil used for over a decade. After bench and phantom tests, the new endorectal coil was applied in patient studies for mpMRI-TRUS guided fusion prostate biopsies with hyperpolarized C-13 pyruvate molecular imaging in three patients on active surveillance. The results of this novel approach with the new 13C/1H coil provides an increase in sensitivity, image quality and ultimately supports better detection of lesions.
Motivation & Goals:
Accurate histopathologic diagnosis and grading of prostate cancer is critical for clinical management of this disease. Currently, transrectal ultrasonography (TRUS)–guided biopsy is considered the standard.1,2,3 However, TRUS is limited for directly visualizing and targeting prostate lesions and therefore the fusion of MR images with US overcomes many of these limitations.1,2 However, conventional anatomic and diffusion MRI does not provide metabolic information on cancer aggressiveness.4,5,6 Recent studies have shown that HP 13C-pyruvate MRI in a rapid 2-minute addition to MRI exams can detect metabolic reprogramming in prostate cancer, improving the detection of aggressive cancers and response to therapy. This project was designed to develop specialized hardware and software to enable multiparametric MR incorporating hyperpolarized (HP) 13C-pyruvate MR molecular imaging for improved MR-US fusion biopsy guidance. In this project, new methods to acquire and display 13C-pyruvate to 13C-lactate conversion rate constants (kPL) images were developed and applied for guiding MR-US fusion biopsies in prostate cancer patients for the first time. The original 13C/1H endorectal coil (ERC) has been used for establishing the safety & feasibility of HP 13C-prostate MRI for detecting aggressive prostate cancers based on significantly higher HP 13C-kPL7,8,9,11 and recently to guide biopsies in larger clinical trials. Using our original 13C/1H endorectal coil design, the first human HP 13C MR clinical trial of 31 patients not only showed safety and feasibility but also the detection of occult prostate cancer.8 While the original 13C/1H endo coil has been used in hundreds of prostate cancer patient exams and has helped improve resolution to 0.34cm3, it is limited by suboptimal geometry with the probe head being too large and the neck too short, residual coupling during transmit, and older preamps & electronics. The original endo coil is also sub-optimal in terms of SNR, ease of use, performance, and robustness. The new endo coil was designed to address these prior limitations and enable new clinical trials applying HP 13C MRI to improve prostate cancer clinical management.Materials & Methods:
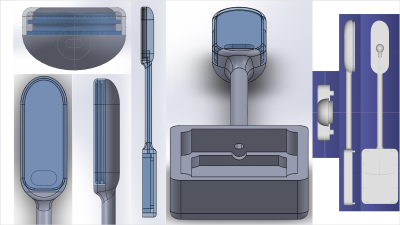
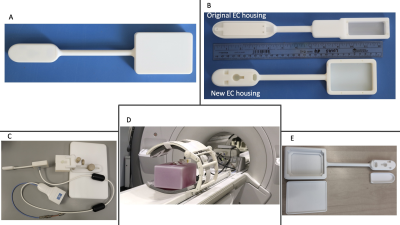
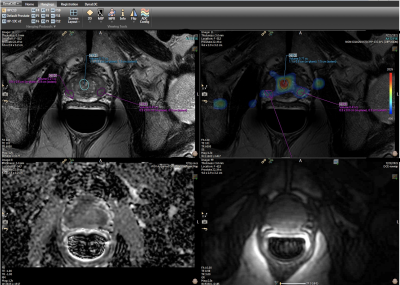
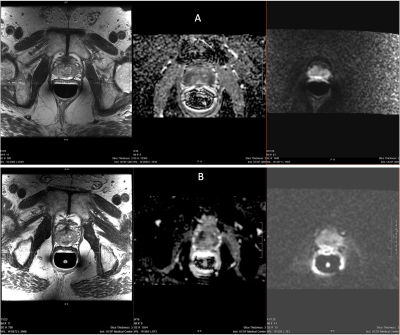
To obtain the highest sensitivity HP 13C & 1H MRI data, a new dual-element endo coil was developed to better detect aggressive prostate cancers within the prostate.7,8,9 Computer design software (SolidWorks) (Figure 1) and commercial 3D printing (Figure 2) was utilized to develop the new ER probe contoured to anatomy with tolerability and size similar to the transrectal ultrasound (TRUS) probes used for biopsy guidance in these patients. With this approach, all mechanical details were 3D-modeled and 3D-printed faster and at lower cost compared to the extensive machine shop milling in making the original endo 13C/1H coil.10 Currently, three patients have been studied with this coil, one of which had also been scanned using the original endo coil 1 year before. As shown in the figures 4 & 5, this subject was previously diagnosed with biopsy-confirmed localized intermediate risk prostate cancer with Gleason 3+4 disease and PSA of 7.5. The 13C scan was acquired with 8mm isotropic (0.5cm3 volumetric) EPI imaging with 2s temporal resolution. The images were reconstructed using Orchestra toolbox (GE) and kPL was calculated using a two-site exchange model6. The kPL images were then uploaded onto PACS and an experienced radiologist outlined HP 13C-kPL targets on Dynacad.Results & Discussion:
The new 13C/1H endo-coil (ERC) (Figure 1 and 2) provided improved patient comfort/tolerance as compared to the prior design and demonstrated substantially improved 13C and 1H MRI sensitivity, with negligible RF coupling in bench electronic testing. Phantom performance testing of new ERC showed a 1.4-1.8-fold improvement in SNR compared to the original ERC.10 As shown in Figure 4 &5, images from a patient study demonstrated not only feasibility for guiding HP 13C mpMR-TRUS fusion biopsies, but also improvements in quantitative measures including signal-to-noise ratios (SNR) and coverage. This patient was scanned using the older endo coil and the new endo coil over a time span of about 1 year. Qualitative and quantitative comparisons of the data acquired showed an improvement in SNR using the new ERC. The results from the new coil on the same patient (Figure 4 & 5) showed substantial improvement with SNR greater than the phantom of 1.8-fold. It is important to note that in addition to the new coil performance, other factors such as polarization and time to injection could have played a role in the SNR improvement in the patient. Three kPL targets were identified in this case (Figure 3), one of which aligned with the standard PIRADs and PSMA-PET lesion. The other two high kPL targets did not have PIRADS correlation, indicating that HP 13C kPLvalues can provide unique metabolic information not depicted by conventional proton imaging for guiding biopsies.Conclusion:
This novel approach with the new 13C/1H ERC provided a substantial increase in SNR and demonstrated the feasibility for enhancing HP 13C mpMR-TRUS fusion biopsies using kPL maps for identifying aggressive cancers acquired as a 2-minute addition to standard-of-care MRI prostate exams.Acknowledgements
This work was supported by grants from the NIH (U01CA232320, U01EB026412, and P41EB013598).References
1. Yacoub JH, Verma S, Moulton JS, Eggener S, Aytekin O. Imaging-guided prostate biopsy: conventional and emerging techniques. Radiographics. 2012 May-Jun;32(3):819-37. doi: 10.1148/rg.323115053. PMID: 22582361.
2. Norberg M, Busch C, Stavinoha J, Scardino PT, Magnusson A. Transrectal ultrasound-guided core biopsies of the prostate. A comparison between the standard 1.2-mm needle and three thinner needles. Acta Radiol. 1994 Sep;35(5):463-7. PMID: 8086255.
3. Norberg M. Transrectal ultrasound and core biopsies for the diagnosis of prostate cancer. A study of pretreatment investigation strategy for patients with suspected prostate cancer. Acta Radiol Suppl. 1994;393:1-21. PMID: 8184698.
4. Gordon JW, Chen HY, Autry A, et al. Translation of Carbon-13 EPI for hyperpolarized MR molecular imaging of prostate and brain cancer patients. Magn Reson Med. 2019;81(4):2702-2709. doi:10.1002/mrm.27549.
5. Chen HY, Larson PEZ, Bok RA, et al. Assessing Prostate Cancer Aggressiveness with Hyperpolarized Dual-Agent 3D Dynamic Imaging of Metabolism and Perfusion. Cancer Res. 2017;77(12):3207-3216. doi:10.1158/0008-5472.CAN-16-2083.
6. Larson PEZ, Chen HY, Gordon JW, et al. Investigation of analysis methods for hyperpolarized 13C-pyruvate metabolic MRI in prostate cancer patients. NMR Biomed. 2018;31(11):e3997. doi:10.1002/nbm.3997
7. Gawlitza J, Reiss-Zimmermann M, Thörmer G, et al. Impact of the use of an endorectal coil for 3 T prostate MRI on image quality and cancer detection rate. Sci Rep. 2017;7:40640. Published 2017 Feb 1. doi:10.1038/srep40640
8. Ganie FA, Wani MS, Shaheen F, et al. Endorectal coil MRI and MR-spectroscopic imaging in patients with elevated serum prostate specific antigen with negative trus transrectal ultrasound guided biopsy. Urol Ann. 2013;5(3):172-178. doi:10.4103/0974-7796.115741
9. Dhatt R, Choy S, Co SJ, Ischia J, Kozlowski P, Harris AC, Jones EC, Black PC, Goldenberg SL, Chang SD. MRI of the Prostate With and Without Endorectal Coil at 3 T: Correlation With Whole-Mount Histopathologic Gleason Score. AJR Am J Roentgenol. 2020 Jul;215(1):133-141. doi: 10.2214/AJR.19.22094. Epub 2020 Mar 11. PMID: 32160050.
10. Nelson SJ, Kurhanewicz J, Vigneron DB, Larson PEZ, Harzstark AL, Ferrone M, van Criekinge M, Chang JW, Bok R, Park I, Reed G, Carvajal L, Small EJ, Munster P, Weinberg VK, Ardenkjaer-Larsen JH, Chen AP, Hurd RE, Odegardstuen L-I, Robb FJ, Tropp J, Murray JA. Metabolic Imaging of Patients with Prostate Cancer Using Hyperpolarized [1-13C]Pyruvate. Science Translational Medicine. 2013; 5(198):198ra108. PMCID: PMC420104
11. Turkbey B, Merino MJ, Gallardo EC, et al. (2014) Comparison of endorectal coil and nonendorectal coil T2 W and diffusion-weigh- ted MRI at 3 Tesla for localizing prostate cancer: correlation with whole-mount histopathology. J Magn Reson Imaging 39(6):1443– 1448. doi:10.1002/jmri.24317
Figures