1047
Optimization of a breast EPI-DWI protocol with high b-values and anterior-posterior phase-encoding direction: initial results1Radiology, University of California, San Diego, La Jolla, CA, United States, 2GE Healthcare, University of California, San Diego, La Jolla, CA, United States, 3National Institute of Standards and Technology, Boulder, CO, United States, 4Bioengineering, University of California, San Diego, La Jolla, CA, United States
Synopsis
Diffusion-weighted imaging (DWI) acquired with echo-planar imaging (EPI) is utilized in breast MRI protocols to evaluate cancer lesions. While clinical implementation is limited by the distortion artifacts which affect EPI, methods such as reverse polarity gradient (RPG) and data collection with reduced field-of-view (FOV) have been used to reduce distortion. Evaluating these methods in minimizing distortion for images acquired with parallel imaging (PI) is a promising approach to improve EPI-DWI breast imaging. Here, we evaluated the distortion magnitude of EPI-DWI data collected with and without PI on a breast phantom and tested the feasibility of this protocol in vivo.
Introduction
Breast MRI is used for pre-operative evaluation, screening and to assess treatment response1. Diffusion weighted imaging (DWI) has been incorporated into breast MRI protocols because of its utility in assessing response and identifying lymph nodes2. DWI is typically acquired with echo-planar imaging (EPI), which is susceptible to distortion artifacts induced by B0-inhomogeneities.Reverse polarity gradient (RPG) is a retrospective approach to correct distortions by exploiting the symmetry of the artifact in the forward and reverse phase encoding (PE) trajectories3. Previously, we characterized the distortion magnitude in EPI-DWI and evaluated RPG’s performance in correcting distortion artifacts4. We found that residual distortions were most prominent in the nipple region when EPI-DWI were collected with PE field-of-view (FOV) oriented left-right (LR). Further, distortion in that region was less pronounced when data were collected in the anterior-posterior (AP) direction, which is typically avoided to minimize breathing and cardiac motion artifacts.
A limitation of previous work was that parallel imaging (PI) was not used, which is commonly available. Thus, in the present work we: (1) characterized the distortion magnitude with and without PI using a breast phantom on EPI-DWI data with PE along anterior-posterior (AP) direction, and (2) tested the feasibility of collecting breast EPI-DWI data in vivo with this protocol.
Methods
A breast phantom5 was scanned using a 3T MRI scanner (GE Healthcare, USA) and 8-channel breast array. Imaging parameters: T1-weighted fat-suppressed spoiled gradient recalled echo (SPGR)— TE/TR=2.7/5.6ms, FA=15°, FOV=360×360mm2, acquisition matrix=512×400, voxel size=0.7×0.7×2.4mm3; high b-value EPI-DWI — TE/TR=86/5500ms, FOV=360×360mm2, acquisition matrix=180×180, voxel size=1.4×1.4×3mm3, maximum b-value=3000 s/mm2, PE direction=AP, and collected without and with PI (factor=2). All EPI-DWI data were distortion corrected using RPG (Figure 1).One side of the breast phantom contains a polycarbonate plate with 84 circles of varying diameter (1-10mm). Regions of interest (ROIs) were manually placed in the center of each circle on structural and DWI data (Osirix, Pixmeo, Switzerland). The spatial discrepancy between the circle centers with respect to the structural images was measured to quantify the distortion magnitude. ROIs over each circle and a background ROI were also drawn to estimate the signal-to-noise ratio (SNR) on EPI-DWI b=0 s/mm2 images.
To test the feasibility of performing EPI-DWI with PE FOV along the AP direction, we collected data using the high b-value EPI-DWI sequence described above and the clinical standard DWI protocol at our institution (below), in three healthy volunteers. Clinical EPI-DWI— TE/TR=58/4000ms, FOV=360×360mm2, acquisition matrix=128×128, voxel size=1.4×1.4×5mm3, maximum b-value=800 s/mm2, PE direction=AP.
Two-way repeated measures analysis of variance (RM-ANOVA) and post-hoc tests were used to evaluate the effects of PI and distortion correction on distortion magnitude in phantom data.
Results
The distortion magnitude was ~50% less when PI was used (5.7±3.2 versus 10.3±5.8mm; p<0.05), and RPG reduced the distortions in both datasets (p<0.05). Residual distortion was larger (p<0.05) in the dataset collected without PI (7.2±5.3 versus 2.6±1.8mm). The images with least distortion (p<0.05) were those collected with PI and corrected with RPG. Distortion magnitude varied across the phantom structure and was largest posteriorly and laterally (Figure 2).The SNR was on average 17.1±15.0% lower on data collected with PI. SNR also varied across the phantom and was lower in the posterior and lateral regions (Figure 3). None of the 1 and 2 mm diameter circles were observable on DWI data collected with or without PI.
Finally, we tested the feasibility of collecting EPI-DWI data with PE direction along AP in vivo (Figure 4). The overall magnitude of the distortion in the nipple was reduced compared to the clinical DWI protocol, which facilitated its correction with RPG. No respiratory or cardiac motion artifacts were observed on the breast tissue on these data.
Discussion and Conclusions
Results suggest that the combination of EPI-DWI data collected with PI and RPG minimizes the magnitude of the distortion caused by B0-inhomogeneities. Residual artifacts were larger in regions with initially more pronounced distortions (posterior and lateral).In DWI, SNR is strongly dependent on the extent of diffusion-weighting. Our SNR results in the breast phantom suggest that our high b-value protocol (bmax=3,000 s/mm2) yields an average SNR of 17.0±6.7 that varied across the FOV. Although no consensus has been reached on the requirements to accurately measure DWI estimates in breast6, an SNR >20 has been suggested to be adequate7. Therefore, future work will involve further optimization of our protocol to ensure minimum SNR of 20 is achieved.
Another finding was that circles in the breast phantom plate with diameter <4mm were not discernable throughout the FOV in our DWI data. This result suggests that the size of the smallest lesion detectable using this protocol may be approximately 4mm in diameter.
In this work, we demonstrated the feasibility of collecting EPI-DWI data with PE direction along AP. This strategy aimed to make the distortion magnitude near the nipple region comparable to the rest of the breast comparable throughout the FOV, such that it may be corrected with RPG. Although the DWI protocol still requires optimization regarding SNR, its lower distortion magnitude and ability to be corrected by RPG are promising.
Acknowledgements
GE Healthcare, Krueger v. Wyeth research awardReferences
1. Shi RY, et al. Breast Lesions: Diagnosis Using Diffusion Weighted Imaging at 1.5T and 3.0T-Systematic Review and Meta-analysis. Clin Breast Cancer. 2018;18:e305-e320.
2. Kim SH, et al. Diffusion-weighted imaging of breast cancer: correlation of the apparent diffusion coefficient value with prognostic factors. J Magn Reson Imaging. 2009;30:615-20.
3. Holland D, Kuperman JM, Dale AM. Efficient correction of inhomogeneous static magnetic field-induced distortion in Echo Planar Imaging. Neuroimage, 2010;50:175-83.
4. Rodríguez-Soto AE, et al. Correction of Artifacts Induced by B(0) Inhomogeneities in Breast MRI Using Reduced-Field-of-View Echo-Planar Imaging and Enhanced Reversed Polarity Gradient Method. J Magn Reson Imaging. 2021;53:1581-1591.
5. Keenan KE, et al. Design of a breast phantom for quantitative MRI. J Magn Reson Imaging. 2016;44:610-9.
6. Baltzer P, et al. Diffusion-weighted imaging of the breast-a consensus and mission statement from the EUSOBI International Breast Diffusion-Weighted Imaging working group. Eur Radiol. 2020;30:1436-1450.
7. Celik A. Effect of imaging parameters on the accuracy of apparent diffusion coefficient and optimization strategies. Diagn Interv Radiol. 2016;22:101-7.
Figures
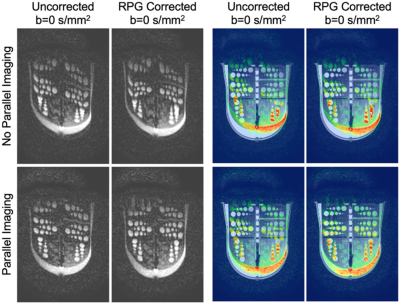
Figure 1. DWI images with and without parallel imaging, before and after distortion correction with RPG. They are also shown overlaid on structural images to show differences in distortion magnitude.
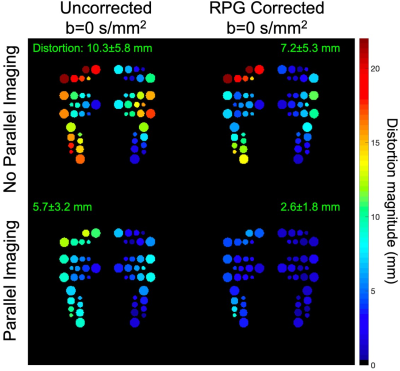
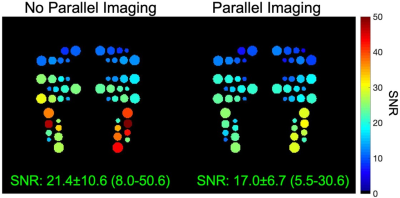
Figure 3. Signal-to-noise ratio (SNR) variation across the breast phantom on data collected with and without parallel imaging. Circles that are not shown are those that weren’t visible on DWI data.
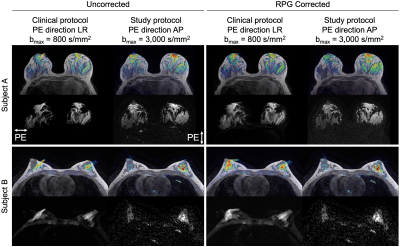
Figure 4. EPI-DWI b=0 s/mm2 images of two volunteers collected using our institution’s clinical DWI protocol (PE direction LR) and a high b-value DWI protocol (PE direction AP), before and after distortion correction with reverse polarity gradient (RPG). Overlaid data are the b=0 s/mm2 images of each DWI sequence.