1017
Association between lesion locations and depressive symptoms in acute stroke patients using voxel-based lesion-symptom mapping1The First Affiliated Hospital of University of Science and Technology of China, Hefei, China, 2Jinling Hospital, Nanjing, China, 3GE Healthcare, Shanghai, China, 4Nanjing First Hospital, Nanjing, China
Synopsis
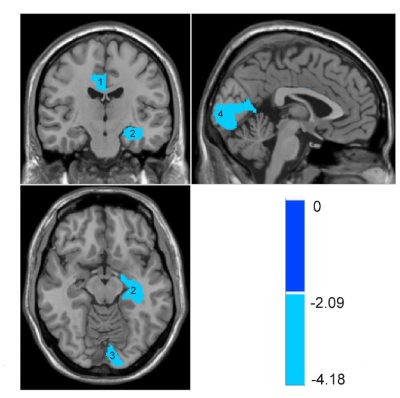
Post-stroke depression (PSD) is a common neuropsychiatric symptom after stroke. The purpose of this study was to investigate the association between lesion locations of brain stroke and PSD occurrence using Voxel-based Lesion-Symptom Mapping (VLSM). VLSM analysis identified clusters within anterior cingulate gyrus, left hippocampus, left lingual lobe where lesions were significantly associated with PSD. The lesion location showed the promise to be used as an independent risk factor of PSD in patients with acute ischemic stroke.
Purpose
Post-stroke depression (PSD) is a common neuropsychiatric symptom after stroke.1 PSD seriously affects the brain function recovery and increases long-term mortality.2 PSD patients usually use antidepressant drugs to relieve symptoms, which may not be effective for all patients. In addition, it remains controversial whether the use of antidepressant drug will increase long-term mortality.3 Therefore, it is of great clinical importance to understand the PSD pathogenesis and improve the treatment effect. Several known risk factors for PSD include gender, age, degree of disability, social support, pre-stroke depression and lesion location. It remains unclear about the relationship between PSD and lesion location of brain stroke. Most of recent studies identified lesion locations by direct observation, which might be inaccurate for small and scattered lesions. Voxel-based Lesion-Symptom Mapping (VLSM) is a new image analysis technique, which investigates the association of cognitive behavior with brain anatomy at the voxel level.4 The purpose of this study was to investigate the association between lesion locations of brain stroke and PSD occurrence at the voxel level.Methods
All the subjects gave written informed consent to participate the study, which was approved by the local ethical committee. A total of 243 acute stroke patients were admitted from the Department of Neurology, First Affiliated Hospital of University of Science and Technology of China (USTC) between September 2020 to March 2021. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) criteria, the patients were divided into PSD and non-PSD groups. The 24-item Hamilton Rating Scale (HAMD) was used to evaluate the severity of depression. MRI examinations were performed within 72 hours of stroke onset, including 3D T1 weighted, T2 weighted, DWI and FLAIR images using a 3.0-T MR750w scanner (GE Healthcare, Milwaukee, WI). Acute infarct lesions on the DWI images were manually segmented using ITK-SNAP software to make a lesion mask. The lesion mask was then applied to the 3D T1 weighted image, which was registered to the standard MNI152 template using the RegLSM toolbox. The results of lesion registration were verified by an experienced radiologist. A lesion distribution probability map was developed in the standard space to perform the following VLSM analysis using NiiStat toolbox. The whole brain was divided into 116 regions based on the Anatomical Automatic Labeling (AAL) template. Liebermeister and Brunner-Munzel were used to correlate PSD occurrence with HAMD scores. Multiple comparisons was performed using Bonferroni correction (corrected P<0.05).Results
In our study, the average age of stroke patients was 58.3 ± 14.8 years and the prevalence of PSD was 28.8% (n=70). Univariate analysis showed that there was a significant difference in Hamilton Anxiety (HAMA) scores between PSD and non-PSD groups. VLSM analysis identified clusters within anterior cingulate gyrus, left hippocampus, left lingual lobe where lesions were significantly associated with PSD (Fig. 1). In addition, the severity of PSD was correlated with the damage in anterior cingulate gyrus, left hippocampus, left lingual lobe and pericalcarine cortex (Fig. 2).Discussion and Conclusion
This study used the VLSM analysis to investigate the association between the PSD occurrence and severity and the lesion locations of brain stroke. The hippocampus and the anterior cingulate gyrus are part of the limbic system and the key components for processing emotions in the brain. The destruction of these structures may lead to the occurrence and progress of depression. The lesion location showed the promise to be used as an independent risk factor of PSD in patients with acute ischemic stroke.Acknowledgements
No acknowledgement found.References
1. Villa RF, Ferrari F, Moretti A. Post-stroke depression: Mechanisms and pharmacological treatment. Pharmacol Ther. 2018;184:131-144.
2. Cai W, Mueller C, Li YJ, et al. Post stroke depression and risk of stroke recurrence and mortality: A systematic review and meta-analysis. Ageing Res Rev. 2019;50:102-109.
3. Paolucci S. Advances in antidepressants for treating post-stroke depression. Expert Opin Pharmacother. 2017;18(10):1011-1017.
4. Bates E, Wilson SM, Saygin AP, et al. Voxel-based lesion-symptom mapping. Nat Neurosci. 2003;6(5): 448-450.