0940
Evaluation of Multiparametric Magnetic Resonance Imaging to assist Adaptive Radiotherapy in Prostate Cancer – an interim report1Radiotherapy Physics, Mount Vernon Cancer Centre, Northwood, United Kingdom, 2Paul Strickland Scanner Centre, Mount Vernon Cancer Centre, Northwood, United Kingdom, 3Mount Vernon Cancer Centre, Northwood, United Kingdom, 4The Christie NHS Foundation Trust and Division of Cancer Services and University of Manchester, Manchester, United Kingdom
Synopsis
Initial results of a prostate cancer study investigating whether multiparametric MRI (MP-MRI), involving diffusion-weighted (DW) and dynamic contrast-enhanced (DCE) MRI, can predict or assess tumour response to radiotherapy (RT) and potentially support adaptive radiotherapy for high-risk patients. Adaptive radiotherapy is a treatment technique utilised to minimise radiation related toxicity. For some cancers it is possible to adapt radiotherapy according to physical changes that occur during treatment. This is not appropriate for prostate cancer treatment since observable changes are generally due to rectal movement, however it may be possible to use multiparametric MRI (MP-MRI) to measure treatment response.
Introduction
Adaptive radiotherapy involves amending the radiation delivered during a radiotherapy course to account for changes in anatomy. Whilst this is not appropriate for prostate cancer treatment, since anatomical changes are primarily due to rectal movement, it may be possible to use multiparametric MRI (MP-MRI) to measure treatment response. This feasibility study investigated whether MP-MRI, involving diffusion-weighted (DW) and dynamic contrast-enhanced (DCE) MRI, can predict or assess response to external beam radiotherapy and potentially support adaptive radiotherapy for high-risk prostate cancer. The study was separated into three complementary aspects: (1) investigation of the effect that neoadjuvant androgen deprivation therapy (ADT) has on the DW-MRI apparent diffusion coefficient (ADC) and the pharmacokinetic DCE-MRI parameters, Ktrans, kep, and IAUGC60; (2) exploration of whether MP-MRI acquired before or during radiotherapy can assess or predict treatment response; (3) assessment of how radiotherapy could be adapted to escalate the dose delivered to a non-responding tumour.Methods
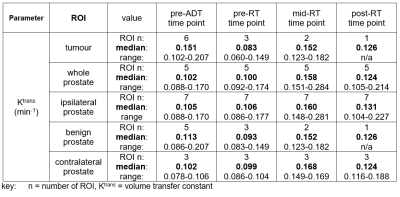
The full study, with UK Health Research Authority ethics approval, will recruit fifteen patients. To date five patients, bringing six tumours, diagnosed with high-risk prostate cancer and referred for neoadjuvant ADT and radiotherapy were prospectively recruited to have MP-MRI examinations before ADT and before, during and after radiotherapy (Fig 1). All MRI data was pseudonymised and information from T2W, DW, T1W DCE images and ADC maps were used by a consultant radiologist to delineate tumour regions of interest (ROI) where the tumour was distinguishable. As it was not always possible to identify tumour on the MP-MR images following ADT, up to five ROIs were contoured: whole prostate; tumour; benign prostate created by subtracting the tumour contour from the whole prostate contour; ipsilateral and contralateral prostate, created by bisecting the whole prostate contour (Fig 2). Reproducibility of the MP-MRI parameters, calculated using Bland-Altman methodology was used to indicate statistically significant changes1-, 5. Comparison was made of MP-MRI parameters (1) between pre-ADT and pre-radiotherapy and (2) between pre-radiotherapy, during-radiotherapy and post-radiotherapy MRI scans. These were analysed using Bland-Altman and one-way analysis of variance (ANOVA). (3) Clinical RT plans used for treatment were adapted by (i) incorporating a simultaneous integrated boost (SIB) for the whole treatment and (ii) by introducing a second treatment phase to escalate the tumour dose to 83Gy, (i) and (ii) were repeated for 90Gy tumour dose escalation.Results
(1) Reproducibility compared favourably to data in the literature1-5 providing confidence in the results. Differences in parameters between cancerous and non-cancerous tissue were observed (Figs 3, 5). All baseline DCE-MRI parameters were higher for tumour ROI than ROIs containing normal tissue, ADC showed the reverse (Fig 3). Statistically significant changes were seen following ADT for several parameters and ROIs.(2) For all ROI the median Ktrans (Figs 4 & 5), kep and IAUCG60 values were lowest before radiotherapy and highest during radiotherapy, the direction of change in median ve at the mid-RT and post-RT MP-MRI varied between ROI, and the median ADC generally increased at subsequent MP-MRI scans. Statistically significant changes were measured in Ktrans (Fig 4), kep kep and ve.
(3) Adaptive planning using both the incorporated dose boost and two-phase techniques to escalate the tumour dose to 83 Gy and 90 Gy was possible without significantly exceeding organ at risk (OAR) dose constraints.
Discussion
The pre-ADT baseline values demonstrate clear differences in parameters between cancerous and non-cancerous tissue. The DCE-MRI parameters, Ktrans, kep, ve and IAUGC60 are higher for the tumour ROI than for ROIs containing normal tissue, whilst the DW-MRI parameter, ADC, is higher for normal tissue. These findings are in keeping with the literature and the baseline values measured in this study agree well with published data. One-way analysis of variance of MRI parameter readings indicated that statistically significant differences between ROIs are only measurable for ve and ADC before therapy has commenced. These interim results suggest that neoadjuvant androgen hormone therapy and radiotherapy are efficacious for a substantial proportion of patients. 67% of the initial tumours could no longer be identified by an experienced radiologist on MP-MR images acquired mid-radiotherapy however this study demonstrated that statistically significant changes were measurable following ADT and radiotherapy for several dynamic MRI parameters. If MP-MRI examinations are able to predict or determine that the dominant intraprostatic lesion will not fully respond to the standard radiotherapy dose prescription, adaptive planning to escalate the dose is feasible. It is likely that the success of plan adaption by dose escalation, with both the simultaneous integrated boost and two-phase approaches, will vary with size and location of the original malignant lesion.Conclusion
These early results suggest that it may be feasible to predict or measure poor high-risk prostate tumour response to neoadjuvant androgen deprivation therapy and radiotherapy using MP-MRI. Subsequent adaption of the radiotherapy plan to deliver an increased tumour dose with the aim of improving outcome also appears to be possible.Acknowledgements
Mount Vernon Cancer Centre Research Award.References
1 Galbraith, S.M., Lodge, M.A., Taylor, N.J., Rustin, G.J.S., Bentzen, S., Stirling, J.J. and Padhani, A.R. (2002). Reproducibility of dynamic contrast-enhanced MRI in human muscle and tumours: Comparison of quantitative and semi-quantitative analysis. NMR in Biomedicine, 15(2), pp.132–142.
2 Padhani, A.R., Hayes, C., Landau, S. and Leach, M.O. (2002). Reproducibility of quantitative dynamic MRI of normal human tissues. NMR in Biomedicine, 15(2), pp.143–153.
3 Lankester, K.J., Taylor, J.N., Stirling, J.J., Boxall, J., D'Arcy, J.A., Collins, D.J., Walker-Samuel, S., Leach, M.O., Rustin, G.J.S. and Padhani, A.R. (2007). Dynamic MRI for imaging tumor microvasculature: Comparison of susceptibility and relaxivity techniques in pelvic tumors. Journal of Magnetic Resonance Imaging, 25(4), pp.796–805.
4 Alonzi, R., Taylor, N. J., Stirling, J.J., D'Arcy, J.A., Collins, D.J., Saunders, M.I., Hoskin, P.J. and Padhani, A.R.. (2010). Reproducibility and correlation between quantitative and semiquantitative dynamic and intrinsic susceptibility-weighted MRI parameters in the benign and malignant human prostate. Journal of Magnetic Resonance Imaging, 32(1), pp.155–164.
5 Rata, M., Collins, D.J., Darcy, J., Messiou, C., Tunariu, N., Desouza, N., Young, H., Leach, M.O. and Orton, M.R. (2016). Assessment of repeatability and treatment response in early phase clinical trials using DCE-MRI: comparison of parametric analysis using MR- and CT-derived arterial input functions. European Radiology, 26(7), pp.1991–1998.
Figures
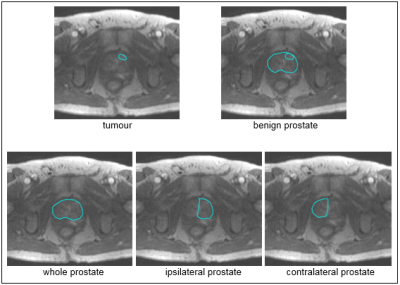
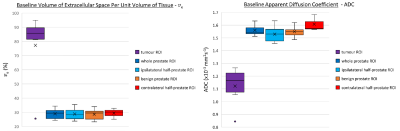
Fig 3. Box plots showing ve (left) and ADC (right) values in tumour, whole prostate, ipsilateral prostate, benign prostate and contralateral prostate ROI at the pre-ADT baseline MRI scan. The boxes show the lower and upper quartiles and the median, the x indicates the mean, the whiskers indicate 1.5x the interquartile range and the dots (•) display outliers.
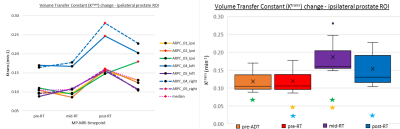
Fig 4. Changes in Ktrans before ADT and before, during and after radiotherapy for ipsilateral prostate ROI.
left: red data points = statistically significant change, black points = non-significant change compared to pre-ADT baseline determined using Bland-Altman methodology
right: boxes show lower, upper and median quartiles, x = mean, whiskers = 1.5x the interquartile range, dots display outliers, stars identify statistically significant differences between green: pre-ADT and mid-RT, yellow: pre-RT and mid-RT, blue: pre-RT and post-RT values determined using one-way ANOVA.