0937
Magnetic Resonance Elastography As a Marker for Prediction of Hepatocellular Carcinoma in Patients with HBV-Related Decompensated Cirrhosis1Department of Radiology, The Third Affiliated Hospital, Sun Yat-Sen University (SYSU), No. 600, Tianhe Road, Guangzhou, Guangdong 510630, People’s Republic of China, Guangzhou, China, 2Department of Radiology, Mayo Clinic College of Medicine, Mayo Clinic, Rochester. MN. USA, Rochester, MN, United States
Synopsis
Hepatitis B virus (HBV)-related decompensated cirrhosis is well-known risk factor for developing hepatocellular carcinoma (HCC). Therefore, it is critical to assess the risk of developing HCC in these patients. Magnetic resonance elastography (MRE) has promise in predicting future events in many chronic liver diseases, but its prognostic role in predicting HCC development of HBV-related decompensated cirrhosis remains unclear. In our study, we evaluated the performance of baseline liver stiffness measurement (LSM) by MRE in predicting HCC development in patients with HBV-related decompensated cirrhosis. Our results showed that MRE-based LSM was associated with HCC development and is independently predictive of HCC development in patients with HBV-related decompensated cirrhosis.
Introduction
Hepatitis B virus (HBV)-related liver cirrhosis is well-known risk factor for developing hepatocellular carcinoma (HCC)[1], especially in patients with decompensated cirrhosis[2]. Therefore, it is of critical importance to assess the risk of developing HCC in patients with HBV-related decompensated cirrhosis for making further optimal surveillance and intervention strategies. Magnetic Resonance Elastography (MRE) has been proven to be the most reliable technique for quantitatively assessing liver fibrosis [3,4]. In addition, several recent studies have focused on predicting future events in many chronic liver diseases [5-8], and the results are promising. However, the applicability of the liver stiffness measurement (LSM) with MRE to HBV-related decompensated cirrhosis for predicting of HCC is still unknown. Therefore, the purpose of this study was to evaluate the performance of baseline LSM by MRE in predicting HCC development in patients with HBV-related decompensated cirrhosis.Methods
We retrospectively enrolled 119 patients (mean age, 50 years; range, 22-77 years; 93 men) with HBV-related decompensated cirrhosis who underwent 3D MRE between July 2015 and December 2018. All patients were followed up at least 2 years after MRE. The primary outcome of interest was the development of HCC, which was diagnosed based on pathologic confirmation or LI-RADS v 2018 criteria. Laboratory results within 30 days of MRE were extracted. The serum fibrosis biomarkers-fibrosis index based on four factors (FIB-4) was calculated using the conventional formulas. The acquisition parameters for 3D SE-EPI MRE sequence were as follows: repetition time, 1334 ms; echo time, 51.7–52.8 ms; EPI-shots, 1; matrix 80 × 80; slice thickness, 3.5 mm; slice spacing, 0 mm; FOV: 38.7–44.8 cm; parallel imaging acceleration factor, 2; phase offsets, 3; vibration frequency, 60H. The regions of interest (ROIs) were drawn in the right lobes of the liver using the MRE magnitude, wave, and stiffness images. Then the mean stiffness of each section was recorded, and the mean value of all sections was computed and weighed by the ROI size. The cumulative incidence (CI) of HCC occurrence, was estimated using the Kaplan-Meier method. Predictive factors were evaluated using the Cox proportional hazard regression model.Results
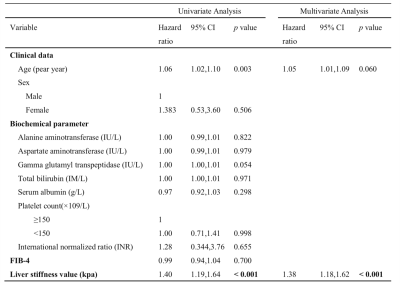
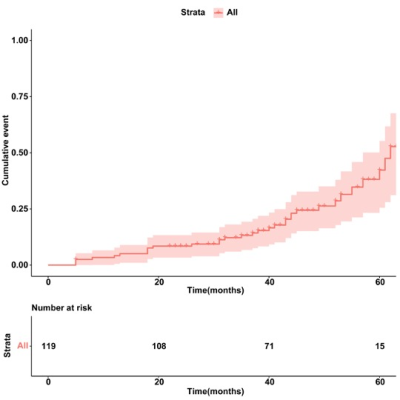
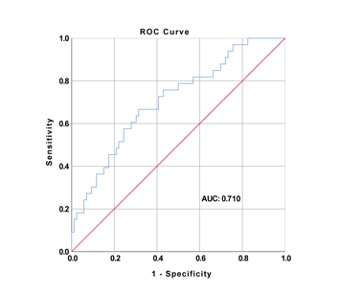
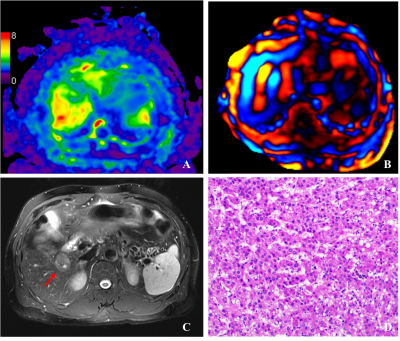
During the follow-up period (median, 44 months [interquartile range, 32–52 months]), 33 patients developed HCC. The 1-, 3-, and 5-year cumulative incidences of HCC were 4.2%, 12.6%, and 18.4%, respectively (Figure1). The baseline median LSM was 5.0kPa, the cut-off of LSM for predicting HCC was 5.36 kPa (AUROC 0.71) (Figure 2). Baseline LSM was predictive of HCC development: age-adjusted HR =1.38 (95% CI, 1.18-1.62, <0.001) per 1 kPa increment (Table 1). Representative MRE image in patient with development HCC are shown in Figure 3. In addition, it showed that FIB-4 model could not independently predict the development of HCC.Discussion
The results of this study showed that LSM by MRE is useful for predicting HCC development in patients with HBV-related decompensated cirrhosis. This approach shows promise for guiding the management of patients who will need high vigilance to capture these outcomes and potentially prevent complications in the future. Limitations of our study include its retrospective design, modest small number of cases, and a follow-up period that was relatively short.Conclusion
In patients with HBV-related decompensated cirrhosis, liver stiffness measured by MRE with a cut-off of ≥5.36 kPa is associated with HCC development, and MRE-based LSM is a significant predictor of future development of HCC.Acknowledgements
The authors state that this study has received funding by the National Natural Science Foundation of China grant 91959118 (JW).References
1. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390(10100):1211-1259.
2. Papatheodoridis GV, Chan HL, Hansen BE, Janssen HL, Lampertico P. Risk of hepatocellular carcinoma in chronic hepatitis B: assessment and modification with current antiviral therapy. J Hepatol 2015;62(4):956-967.
3. Mathew RP, Venkatesh SK. Imaging of Hepatic Fibrosis. Curr Gastroenterol Rep 2018;20(10):45.
4. Lefebvre T, Wartelle-Bladou C, Wong P, et al. Prospective comparison of transient, point shear wave, and magnetic resonance elastography for staging liver fibrosis. Eur Radiol 2019;29(12):6477-6488.
5. Han MAT, Vipani A, Noureddin N, et al. MR elastography-based liver fibrosis correlates with liver events in nonalcoholic fatty liver patients: A multicenter study. Liver Int 2020;40(9):2242-2251.
6. Gidener T, Ahmed OT, Larson JJ, et al. Liver Stiffness by Magnetic Resonance Elastography Predicts Future Cirrhosis, Decompensation, and Death in NAFLD. Clin Gastroenterol Hepatol 2021;19(9):1915-1924 e1916.
7. Gidener T, Yin M, Dierkhising RA, Allen AM, Ehman RL, Venkatesh SK. MRE for Prediction of Long-Term Progression and Outcome in Chronic Liver Disease: A Retrospective Study. Hepatology 2021.
8. Osman KT, Maselli DB, Idilman IS, et al. Liver Stiffness Measured by Either Magnetic Resonance or Transient Elastography Is Associated With Liver Fibrosis and Is an Independent Predictor of Outcomes Among Patients With Primary Biliary Cholangitis. J Clin Gastroenterol 2021;55(5):449-457.
Figures