0928
Comparison of single-shot EPI DWI and multi-shot EPI DWI in prostate MRI
Ayumu Kido1, Akira Yamamoto1,2, Mitsuru Takeuchi3, Yu Ueda4, Jaladhar Neelavalli5, and Tsutomu Tamada1
1Radiology, Kawasaki Medical School, Kurashiki, Japan, 2Radiology, Kawasaki Medical School, Kurashiki-shi, Japan, 3Radiology, Radiolonet Tokai, Nagoya, Japan, 4Philips Japan, Tokyo, Japan, 5Philips India, Bangalore, India
1Radiology, Kawasaki Medical School, Kurashiki, Japan, 2Radiology, Kawasaki Medical School, Kurashiki-shi, Japan, 3Radiology, Radiolonet Tokai, Nagoya, Japan, 4Philips Japan, Tokyo, Japan, 5Philips India, Bangalore, India
Synopsis
Single-shot EPI (sshEPI) DWI still suffers from distortion and blurring. Multi-shot EPI (mshEPI) DWI called IRIS enables to reduce image distortion and blurring. A total of 142 patients with suspected prostate cancer (PC) underwent mpMRI including sshEPI DWI and IRIS under the same scan time. The image quality and diagnostic performance of the lesions were compared between sshEPI DWI and IRIS. IRIS improved image distortion and blurring compared to sshEPI DWI, and also suggested a similar or higher diagnostic performance compared to sshEPI DWI.
Introduction
DWI is key component of multi parametric MRI (mpMRI) in prostate1,2. Single-shot EPI (sshEPI) DWI is the most commonly used in routine clinical examination thanks to high SNR, rapid acquisition, and insensitive to motion. On the other hand, drawbacks are mainly distortion due to B0 inhomogeneity and blurring due to T2* attenuation. Multi-shot EPI (mshEPI) DWI, which acquires the k-space data in multiple excitations, can reduce distortion and blurring due to shorter shot length, whereas it is sensitive to motion due to phase differences between shots. MshEPI DWI called IRIS3, which can compensate for phase shifts between shots by implementing the rejection/reacquisition function, provides robust image quality even in the presence of tissue motion. Therefore, IRIS enables to reduce image distortion and blurring compared to conventional sshEPI DWI. The purpose of this study is to compare sshEPI DWI and IRIS under the same scan time to investigate clinical feasibility of IRIS for prostate cancer (PC).Methods
A total of 142 patients with suspected PC underwent mpMRI at a 3-T system (Ingenia Elition 3.0T; Philips Healthcare, Best, The Netherlands) with a 32-channel phased-array coil. Axial sshEPI DWI and IRIS were acquired with the imaging parameters described in Figure 1. The same parameters were used in this study except for the number of shots, EPI factor, number of signals averaged (NSA), and reduction factor. NSA in sshEPI DWI was optimized so that scan time in sshEPI DWI are the same as that of IRIS. In qualitative assessment, anatomical distortion of prostate (AD, 1=severe; 2=moderate, 3=mild; 4=none), lesion conspicuity score (LCS, 1=invisible for surrounding normal site; 2=slightly high, 3=moderately high; 4=very high), and prostate edge clarity (PEC, 1=very poor; 2=poor, 3=moderate; 4=good) based on 4-point scales by two readers. In quantitative analysis, SNR (SNR= normal prostate SI (mean) / internal obturator muscle standard deviation (SD)) and contrast to noise ratio (CNR= lesion SI (mean) - normal prostate SI (mean) / internal obturator muscle SD) between three acquisition methods were compared. Comparison between lesion apparent diffusion coefficient (ADC) and normal peripheral zone (PZ) ADC, and lesion ADC in PC with GS≤3+4 and lesion ADC in PC with GS≥4+3 in each acquisition method was also performed. In 17 PC patients who underwent prostatectomy, a radiologist assessed eight regions (six peripheral zones (PZ) and two transition zones (TZ) using DWI score in PI-RADS v 2.1 (total 136 regions). To evaluate diagnostic performance of the lesion ADC and the DWI score for clinically significant prostate cancer (csPC) detection, area under the curve (AUC) was calculated. Wilcoxon signed rank test, Mann-Whitney U test, ROC analysis, and DeLong’s test were used for statistical analysis.Results
AD in IRIS was significantly higher than that in sshEPI DWI (3.26±0.75 vs. 3.05±0.78 and 3.67±0.56 vs. 3.30±0.80, P<0.001 in both) in both readers (Figure 2). LCS was significantly higher in IRIS than in sshEPI DWI in reader 1 (3.84±0.42 vs. 3.82±0.50, P=0.025), but not in reader 2 (3.78±0.56 vs. 3.70±0.61, P=0.739) . PEC in IRIS was significantly higher than that in sshEPI DWI in both readers (3.54±0.57 vs. 3.04±0.66 and 3.73±0.48 vs. 2.98±0.84, P<0.001 in both) (Figure 3). SNR and CNR in sshEPI DWI were significantly higher than that in IRIS (37.61±13.31 vs. 18.04±7.09 and 43.63±23.52 vs. 23.36±11.15, P<0.001 in both). Lesion ADC was significantly lower than benign ADC in both sequences (0.69±0.23 vs. 1.59±0.48 in sshEPI DWI and 0.70±0.23 vs. 1.69±0.51 in IRIS, P<0.001 in both). Lesion ADC in PC with GS≥4+3 was significantly lower than that in PC with GS≤3+4 in both sequences (0.75±0.20 vs. 0.64±0.23, P=0.012 in sshEPI DWI and 0.75±0.20 vs. 0.65±0.23, P=0.029 in IRIS). For discrimination ability between PC with GS≤3+4 and PC with GS≥4+3 using lesion ADC, the AUC was comparable between sshEPI DWI and IRIS (0.696 and 0.670, respectively, P=0.560). For diagnostic performance of csPC using DWI score, the AUC in IRIS was comparable to that in sshEPI DWI (0.844 and 0.850, respectively, P=0.650). There were 6 regions with discrepant results between both sequences for csPC detection. Two regions had true positive in IRIS and false negative in sshEPI DWI, 3 regions had true negative in IRIS and false positive in sshEPI DWI, and one lesion had false positive in IRIS and true negative in sshEPI DWI.Discussion
In comparison of the image quality, SNR and CNR were higher in sshEPI DWI than in IRIS under the same scan time, and the image distortion and sharpness such as AD and PEC showed better results in IRIS than in sshEPI DWI in both readers. In comparison of the tumor detection ability in PC, lesion ADC was comparable between both sequences. Although LCS was different between the two readers. For discrimination ability between PC with GS≤3+4 and PC with GS≥4+3 using lesion ADC, the AUC was comparable between both sequences. For diagnostic performance of csPC using DWI score, the AUC in IRIS was comparable to that in sshEPI DWI. However, the discrepant results between both sequences suggest that IRIS has higher diagnostic performance compared to sshEPI DWI (Figure 4).Conclusion
IRIS improved image distortion and blurring compared to sshEPI DWI, and also suggested a similar or higher diagnostic performance compared to sshEPI DWI.Acknowledgements
No acknowledgement found.References
- Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019;76(3):340-351.
- Le Bihan D. Apparent diffusion coefficient and beyond: what diffusion MR imaging can tell us about tissue structure. Radiology. 2013;268(2):318–322.
- Jeong HK, Gore JC, Anderson AW. High-resolution human diffusion tensor imaging using 2-D navigated multishot SENSE EPI at 7 T. Magn Reson Med. 2013;69(3):793-802.
Figures
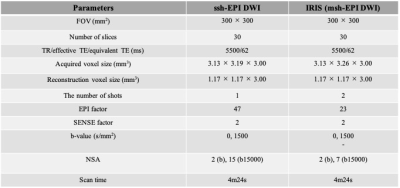
Details of the imaging parameter
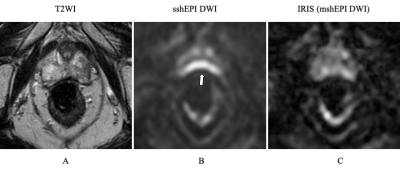
A 79-year-old male with prostate cancer (PSA level of 15.67 ng/mL, Gleason score of 4+3) in the peripheral zone. Cancer lesion is not shown on two DW images. These DW images show distortion of the prostate caused by rectal air. IRIS (C) can reduce rectal gas induced distortion compared to sshEPI DWI (B).
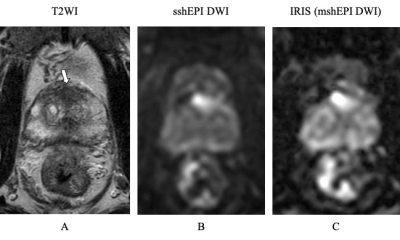
A 80-year-old male with prostate cancer (PSA level of 13.69 ng/mL, Gleason score of 3+4) in the transitional zone. Cancer lesion is shown as a homogeneous hypointense lesion with mass effect on T2-weighted imaging (A). The lesion with focal hyperintensity is depicted clearly in the two DWI image (sshEPI DWI and IRIS) (B, C). SNR and CNR is higher in sshEPI DWI than in IRIS, whereas sharpness in IRIS is better than sshEPI DWI.
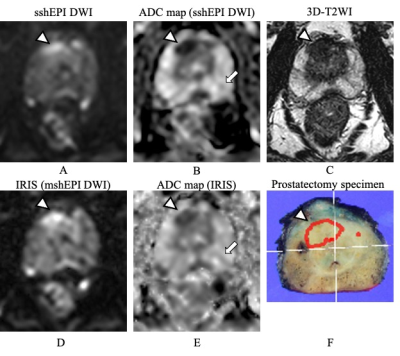
A 72-year-old male with prostate cancer (PSA level of 8.79 ng/mL, Gleason score of 3+4) in the transitional zone (△) (A-F). The ADC map of sshEPI DWI shows a localized slightly hypointense area in the left PZ that is different from the background (→) (B). sshEPI DWI shows no high signal (A). DWI score was assigned as 3 by PI-RADS v2.1. The ADC map of IRIS showed a linear hypointense area, which was assigned a DWI score of 2 (→) (E). No prostate cancer was found in the left peripheral zone in the Prostatectomy specimen (F).
DOI: https://doi.org/10.58530/2022/0928