0926
VERDICT-MRI Analysis of False Positives in Prostate Mp-MRI1Centre for Medical Image Computing, University College London, London, United Kingdom, 2Molecular Diagnostics and Therapeutics Group, University College London, London, United Kingdom, 3Department of Urology, University College London Hospitals NHS Foundation Trust, London, United Kingdom, 4Department of Pathology, University College London Hospitals NHS Foundation Trust, London, United Kingdom, 5Centre for Medical Imaging, University College London, London, United Kingdom
Synopsis
Mp-MRI has moderate specificity for the diagnosis of prostate cancer, resulting in many false positive results and unnecessary biopsies for patients with other prostatic diseases. This work presents an approach using VERDICT-MRI to investigate differences in microstructural parameter estimates between normal prostate tissue, false positive lesions and clinically-significant cancer. The VERDICT intracellular volume fraction and intrinsic diffusivity in the extracellular-extravascular space can discriminate false positive lesions with greater accuracy than the clinical ADC from mp-MRI. These results show VERDICT has the potential to identify false positives and reduce unnecessary biopsies in prostate patients.
Introduction
Multiparametric MRI (mp-MRI) is a standard part of the prostate cancer diagnosis pathway [1], however whilst the technique has 90% sensitivity, its specificity is moderate at only 50% [2]. This results in one in two men undergoing unnecessary biopsy for a suspected cancerous lesion [3], which is either benign or shows clinically insignificant cancer - these cases are referred to as false positives. The Vascular, Extracellular and Restricted Diffusion for Cytometry in Tumours (VERDICT) MRI technique [4] is a non-invasive imaging method that uses a mathematical model along with an imaging protocol to connect the diffusion-weighted (DW) signal to microscopic features of tissues. In comparison to naïve DW-MRI from mp-MRI, the VERDICT acquisition protocol is much richer, allowing for probing of the underlying microstructure to reveal changes in tissue features similar to histology. VERDICT has shown promising results in clinical settings discriminating normal from malignant tissue and grading [5, 6]. In this work, we report on differences in VERDICT parameter estimates between normal prostate tissue, false positive lesions and clinically significant cancer, highlighting the potential to reduce unnecessary biopsies in men with diseases other than cancer.Methods
Patient population: 23 men who were being investigated for suspected prostate cancer were recruited for this study. 11 of these men had lesions with clinically significant cancer (one patient with two lesions), whilst the remaining 12 had other diseases such as atrophy, inflammation or high-grade PIN (confirmed via targeted biopsy).DW-MRI acquisition: All men underwent mp-MRI on a 3T scanner (Achieva, Philips Healthcare, Best, Netherlands). Following this, VERDICT-MRI data for all patients was acquired with a pulsed-gradient spin echo (PGSE) sequence using an optimised imaging protocol for VERDICT prostate characterisation with five b-values (90; 500; 1500; 2000; 3000 s/mm2) in three orthogonal directions. Images with b=0s/mm2 were also acquired before each b-value acquisition. The DWI sequence was acquired with a voxel size of 1:251:255mm3, and the images were reconstructed to a 176x176x14 matrix size [7].
DW-MRI analysis: The VERDICT model for prostate characterises diffusion in the vascular (VASC), extracellular-extravascular space (EES) and intracellular (IC) compartments in tumours. We estimate four model parameters: fIC (IC volume fraction), fEES (EES volume fraction), and fVASC vascular volume fraction where (fVASC=1- fIC-fEES), as well as cell radius R and diffusivity dEES in the extracellular-extravascular space. The DW-MRI signal for VERDICT is:
S(b)/S0 = fVASCSVASC(DVASC, b) + fICSIC(DIC, R, b) + fEESSEES(DEES, b)
where b is the b-value and S0 is the b=0 signal intensity. Specific compartment signal expressions can be found in [4].
Model fitting: The VERDICT model was fitted to the DW-MRI data in each voxel using deep neural networks to produce parametric maps [8, 9]. Specifically, in this work the multi-layer perceptron algorithm was used for ultrafast and robust model fitting [10].
Statistical analysis: Assessment of VERDICT parameters and apparent diffusion coefficient (ADC) in differentiating tissue types was conducted via the Wilcoxon's signed rank test. Performance of VERDICT parameters in comparison to that of ADC (derived from mp-MRI) was also evaluated.
Results
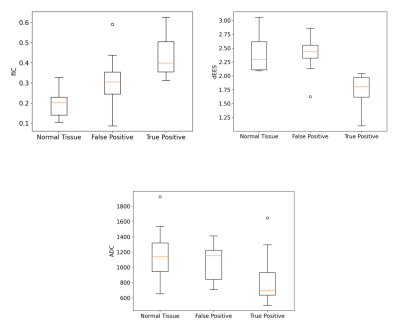
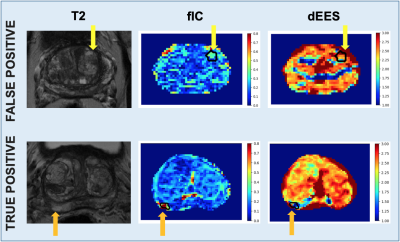
In Figure 1, we observe statistically different values in the VERDICT fIC between normal tissue and false positives (p = 0.02). The rest of the VERDICT parameters do not shoe significant differences between these two tissue types. The VERDICT fIC also has statistically different values in false positive lesions compare to true positives (p = 0.02). In addition, the VERDICT dEES has the most marked differences in mean values between true and false positive lesions (p = 0.001). In comparison, the ADC derived from the mp-MRI did not show statistically different values between normal tissue and false positives. Whilst statistically significant differences were found using the ADC between true and false positives (p = 0.04), the differences in the mean values of the fIC and dEES were more marked.Figure 2 displays examples of VERDICT parametric maps of fIC and dEES alongside a T2-weighted image for a patient with a false positive lesion and a patient with clinically significant cancer. We observe higher fIC values and lower dEES values in true positive lesions than in false positive, along with increased lesion conspicuity using VERDICT maps for both parameters.
Discussion and Conclusion
In this work we use VERDICT-MRI to investigate noninvasively differences in microstructural estimates between false positives, clinically-significant cancer and normal prostate tissue. We found that the VERDICT intracellular volume fraction has statistically different values in normal tissue, false positive and true positive prostate lesions. It achieves this with greater statistical significance than the clinical ADC – this is in agreement with previous work demonstrating that the fIC discriminates between Gleason grades with greater accuracy than ADC [6]. In addition, the ADC cannot discriminate between normal tissue and false positives. The VERDICT extracellular-extravascular diffusivity appears to be a very strong promising marker as it can differentiate between true and false positives with greater accuracy than both ADC and fIC. These results indicate that VERDICT can discriminate false positive lesions with greater accuracy than ADC and has the potential to reduce the number of unnecessary biopsies of prostate patients. Future work will analyse a larger patient cohort, and investigate the use of the VERDICT model that also estimates relaxation [9].Acknowledgements
This work was supported by EP/N021967/1, EP/S021930/1 and by Prostate Cancer UK: Targeted Call 2014: Translational Research St.2, project reference PG14-018-TR2.
References
1. Graham J, Kirkbride P, Cann K, et al. Prostate cancer: summary of updated NICE guidance. BMJ. 2014;348:f7524.
2. Lee SI, Hectors SJ. Prostate MRI: Toward Imaging Tumor Histology. Radiology. 2020;296(2):356-7.
3. Ahmed HU, El-Shater Bosaily A, Brown LC, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389(10071):815-22.
4. Panagiotaki E, Chan RW, Dikaios N, et al. Microstructural Characterization of Normal and Malignant Human Prostate Tissue With Vascular, Extracellular, and Restricted Diffusion for Cytometry in Tumours Magnetic Resonance Imaging. Investigative Radiology. 2015;50(4):218-27.
5. Panagiotaki E, Walker-Samuel S, Siow B, et al. Noninvasive Quantification of Solid Tumor Microstructure Using VERDICT MRI. Cancer Research. 2014;74(7):1902-12.
6. Johnston EW, Bonet-Carne E, Ferizi U, et al. VERDICT MRI for Prostate Cancer: Intracellular Volume Fraction versus Apparent Diffusion Coefficient. Radiology. 2019;291(2):391-7.
7. Eleftheria Panagiotaki, Andrada Ianus, Edward Johnston, Rachel W Chan, Nicola Stevens, David Atkinson, Shonit Punwani, David J Hawkes, and Daniel C Alexander. Optimised verdict mri protocol for prostate cancer char- acterisation. In (Proceedings) International Society for Magentic Resonance in Medicine (ISMRM), 2015
8. V. Valindria, E. Chiou, M. Palombo, S. Singh, S. Punwani, and E. Panagiotaki. Synthetic q-space learning with deep regression networks for prostate cancer characterisation with verdict. In (Proceedings) IEEE International Symposium on Biomedical Imaging (ISBI). IEEE (In press, 2021).
9. Marco Palombo, Vanya Valindria, Saurabh Singh, Eleni Chiou, Francesco Giganti, Hayley Pye, Hayley C. Whitaker, David Atkinson, Shonit Punwani, Daniel C. Alexander, and Eleftheria Panagiotaki. Joint estimation of relaxation and diffusion tissue parameters for prostate cancer grading with relaxation-VERDICT MRI. July 2021.
10. Vladimir Golkov, Alexey Dosovitskiy, Jonathan I. Sperl, Marion I. Men- zel, Michael Czisch, Philipp Samann, Thomas Brox, and Daniel Cremers. q-space deep learning: Twelve-fold shorter and model-free diffusion MRI scans. IEEE Transactions on Medical Imaging, 35(5):1344–1351, May 2016.
Figures