0896
Free-Running 5D Flow MRI: Impact of Cardiac Temporal Resolution on Flow Quantification1Biomedical Engineering, Northwestern University, Evanston, IL, United States, 2Radiology, Feinberg School of Medicine, Chicago, IL, United States, 3Medical Imaging, Lurie Children's Hospital, Chicago, IL, United States, 4Radiology, Lausanne University Hospital (CHUV) and University of Lausanne (UNIL), Lausanne, Switzerland
Synopsis
The flexible reconstruction of 5D flow MRI data may be particularly beneficial in pediatric cases where cardiac cycle length varies greatly. We compared flow measurements from 5D flow and 2D phase contrast. 5D flow data was reconstructed using either a cardiac bin width of 40ms or that matching the 2D phase contrast reconstruction. We find excellent correlation of both 5D flow reconstructions with 2D phase contrast. There is overestimation of arterial flow measures by 5D flow, with most overestimation by the short temporal resolution reconstruction. Further study should additionally compare with 4D flow MRI.
Introduction
Free-running 5D flow MRI is a novel technique that enables fully self-gated cardiac and respiratory motion-resolved measurements of blood flow over a 3D volume. Data acquisition utilizes highly accelerated radial k-space sampling, followed by sorting of k-space lines in flexible user defined cardiac and respiratory bins, and subsequent compressed sensing reconstruction (5D = 3D + cardiac time + respiration). Several previous 5D flow studies have used similar cardiac temporal resolution - approximately 40ms, and 4 respiratory states (end-expiration to inspiration).2-4 However, the impact of the selection of the 5D flow cardiac temporal resolution on the accuracy of flow quantification has not been systemically investigated. Since 5D flow is a useful tool in studying congenital heart disease (CHD), such as single ventricle physiology,1 this may be particularly relevant in young pediatric patients with known higher heart rates. It is thus important to investigate the impact of cardiac phase resolution on flow measurement in the pediatric population. We aimed to investigate whether increasing the temporal resolution in pediatric patients with CHD would improve 5D flow agreement with the clinically standard 2D phase contrast MRI.Methods
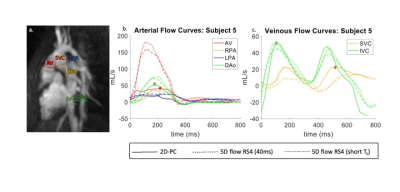
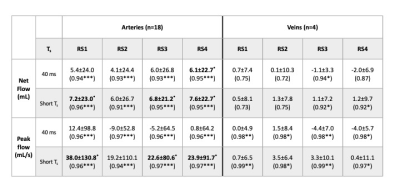
5D flow MRI2 was acquired in 6 patients with CHD who received ferumoxytol during a clinically indicated cardiac MR study. All patients received 2D phase contrast (PC) MRI in at least two vessels. 2D-PC MRI (spatial resolution: 1.1-1.3x1.1-1.3mm, temporal resolution: 16.1-28ms, venc: 80-250cm/s) was acquired over 1 minute during a breath hold if under general anesthesia or free breathing otherwise and the images were retrospectively cardiac gated using EKG (Fig 1a). Each 5D flow dataset (FOV: 150-200x150-200mm, spatial resolution: 1.5mm-2mm isotropic, venc: 150cm/s) was reconstructed twice: once with 40ms cardiac temporal resolution (Ts) and once with a higher temporal resolution, matching that of the 2D-PC MRI reconstructed images (herein called short Ts reconstruction). 2D-PC temporal resolutions are listed in table 1. All 5D-flow reconstructions used 4 respiratory states (RS, Fig 1b). Net flow and peak flow were measured in each vessel with a corresponding 2D-PC MRI measurement (Fig 2a) using commercial software (Circle CVI, Calgary, Canada). Bland Altman analysis was used to assess agreement between 2D-PC and each of the RS bins of 5D flow MRI. Results were reported as percent difference bias ± limits of agreement (LOA). Data was stratified on vessel type (vein/artery).Results
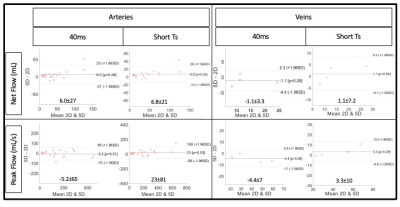
The study cohort (8.7±5.4yrs, 1 female, HR: 91±22 bpm) demographics are described in table 1. Flow curves for subject 5 are shown in figure 2, demonstrating the distinct difference in flow for arterial and venous measurements. In arteries, we found that both 5D flow reconstructions significantly overestimated 2D-PC net flow. Further, the short Ts reconstruction overestimated arterial peak flows in all RS bins (table 2). Correlation of 5D flow with 2D-PC MRI was excellent in arterial measures (R2 > 0.91). In veins, there was no significant bias for any reconstruction or metric. Good correlation was seen in venous measures (net flow: R2> 0.72; peak flow: >0.97). Across both metrics and vessel types, RS3 had the narrowest average LOA for the short Ts 5D flow reconstruction whereas RS2 had the narrowest average LOA for the 40ms reconstruction (table 2). Bland-Altman plots from RS3 are shown in figure 3.When comparing the 5D flow reconstructions, we found that the short Ts reconstruction had an average percent increase of 8.6% in net flow and 10.4% in peak flow. There was excellent correlation between the reconstructions in all bins (R2>0.97).
Discussion
We demonstrate that in a cohort of pediatric CHD patients, 5D flow derived net flow and peak flow had excellent correlation with 2D-PC measurements. Overall, we observed few significant biases in the 40ms reconstruction whereas the short Ts reconstruction generally overestimated arterial flow measures. This overestimation may be due to reduced smoothing in the signal over time or may be due to the compressed sensing (CS) being poorly tuned to reconstruction on cardiac bins with fewer lines of acquired k-space. We also found that RS2 and RS3 had the narrowest LOAs for arterial and venous measures, suggesting that these bins may most closely match the 2D-PC MRI respiratory state. This study was limited by its heterogenous cohort and variable velocity encodes and breathing status during 2D-PC acquisition. Additionally, it faces the inherent challenge of exactly replicating the places from 2D-PC acquisition within the 3D volume of the 5D flow data. Future work should include a larger cohort, emphasizing inclusion of venous measurements, and comparisons to 4D flow MRI.Conclusion
Pediatric patients have a wide range of heart rates, and thus may benefit from the flexible reconstruction of 5D flow MRI to ensure sufficient cardiac phase resolution. We demonstrated that, in a heterogenous cohort of pediatric CHD patients, both standard 40ms and reduced Ts reconstructions had excellent agreement with 2D-PC. However, there is additional significant bias in the short Ts reconstruction compared to the standard 40ms reconstruction. It is unclear if these biases reflect uncaptured flow in the clinical-standard and these differences will require further investigation.Acknowledgements
No acknowledgement found.References
[1] van der Woude, S. F., Rijnberg, F. M., Hazekamp, M. G., Jongbloed, M. R., Kenjeres, S., Lamb, H. J., ... & Wentzel, J. J. (2021). The influence of respiration on blood flow in the Fontan circulation: insights for imaging-based clinical evaluation of the total cavopulmonary connection. Frontiers in Cardiovascular Medicine, 8.
[2] Ma, L. E., Yerly, J., Piccini, D., Di Sopra, L., Roy, C. W., Carr, J. C., ... & Markl, M. (2020). 5D flow MRI: a fully self-gated, free-running framework for cardiac and respiratory motion–resolved 3D hemodynamics. Radiology: Cardiothoracic Imaging, 2(6), e200219.
[3] Falcão, M. B., Di Sopra, L., Ma, L., Bacher, M., Yerly, J., Speier, P., ... & Roy, C. W. (2021). Pilot tone navigation for respiratory and cardiac motion‐resolved free‐running 5D flow MRI. Magnetic resonance in medicine.
[4] Ma, L., Yerly, J., Di Sopra, L., Piccini, D., Lee, J., DiCarlo, A., ... & Markl, M. (2021). Using 5D flow MRI to decode the effects of rhythm on left atrial 3D flow dynamics in patients with atrial fibrillation. Magnetic resonance in medicine, 85(6), 3125-3139.
Figures