0837
68Ga-PSMA and 68Ga-DOTA-RM2 PET/MRI in staging of high-risk prostate cancer patients: Preliminary analysis on 13 patients1Department of Nuclear Medicine, IRCCS San Raffaele Scientific Institute, Milan, Italy, 2Vita-Salute San Raffaele University, Milan, Italy, 3Department of Radiology, IRCCS San Raffaele Scientific Institute, Milan, Italy, 4Department of Urology and Division of Experimental Oncology, URI, Urological Research Institute, IRCCS San Raffaele Scientific Institute, Milan, Italy, 5Department of Pathology IRCCS San Raffaele Scientific Institute, Milan, Italy
Synopsis
The use of PET/MRI scanners is an innovative approach to stage prostate cancer (PCa) and the combined use of both 68Ga-PSMA and 68Ga-DOTA-RM2 radiotracers can improve disease staging by providing different metabolic aspects of the tumour. In the present study, 13 patients with high-risk PCa undergoing 68Ga-PSMA and 68Ga-DOTA-RM2 PET/MRI before radical prostatectomy have been included, with availability of histology as gold standard to validate intraprostatic findings and local extension. Our results suggest that the use of PET/MRI with a dual tracer approach can improve PCa staging, by providing complementary information ameliorating disease characterization.
Introduction
Prostate cancer (PCa) is the second most common cancer in men worldwide1. While histological confirmation is required for the diagnosis of PCa, multi-parametric MRI (mp-MRI) is commonly implemented in the clinical routine to detect the primary tumor, guide biopsies and define the local extent of the disease2,3. PET molecular imaging is another valid imaging approach in PCa staging, with new PET tracers bearing potential to improve diagnosis, staging and follow-up of PCa4–6. Hybrid PET/MRI allows the simultaneous acquisition of metabolic, structural, and functional imaging information concerning PCa status in a whole-body single session examination. The aim of the present study is to investigate the synergic role of 68Ga-PSMA PET, 68Ga-DOTA-RM2 PET and MRI in PCa staging using a hybrid PET/MR scanner.Methods
Thirteen patients (mean age 66.74, sd 8.77) with biopsy-proven PCa underwent 68Ga-PSMA PET/MRI and 68Ga-DOTA-RM2 PET/MRI in two different days for staging purpose. Radical prostatectomy was then performed. The PSMA protocol consisted in a high statistic (HS) pelvic PSMA PET bed, during which T2, DWI, DCE sequences were acquired and a Total Body PET acquisition with LAVA-flex and DWI at each bed. The 68Ga-DOTA-RM2 protocol consisted in a HS pelvic 68Ga-DOTA-RM2 PET bed during which T2 sequence was acquired and Total Body PET acquisition with LAVA-flex. TNM classification based on image findings was performed and quantitative imaging parameters were collected for each scan. Specifically, on the pelvic HS PET beds, VOIs on the tumor lesions were segmented on the 68Ga-PSMA PET, 68Ga-DOTA-RM2 PET and on T2 MR images by an expert Nuclear Medicine physician and an expert radiologist. After having coregistered PSMA and DOTA-RM2 studies, DICE score between VOIs was computed. Furthermore, the histological data derived from prostatectomy were used as gold standard to validate intraprostatic findings as well as local extension of the disease.Results
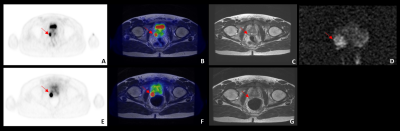
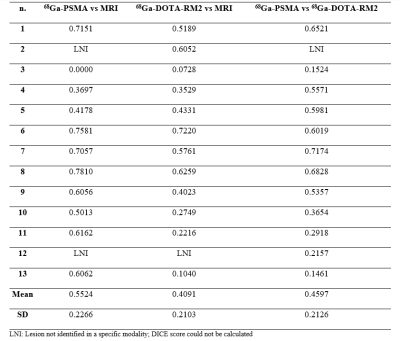
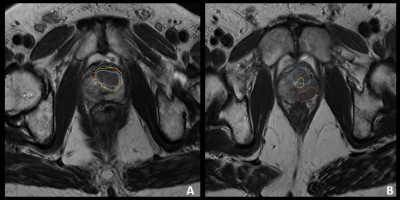
Figure 1 shows an example of study in a 53ys old patient. The analysis of semi-quantitative parameters of prostate uptake extracted from HS 68Ga-PSMA images showed a mean SUVmax of 19.18 (sd: 10.920), SUVmean40-50-60% of 11.597, 12.885, 14.569, respectively (sd: 6.791, 7.587, 8.434, respectively), MTV40-50-60% of 1.613, 1.129, 0.712, respectively (sd: 0.910, 0.813, 0.707, respectively). The analysis of semi-quantitative parameters of prostate uptake extracted from HS 68Ga-DOTA-RM2 images showed a mean SUVmax of 15.323 (sd: 7.827), SUVmean40-50-60% of 9.745, 10.782, 11.54, respectively (sd: 5.204, 5.732, 6.003, respectively), MTV40-50-60% of 2.899, 2.140, 1.664, respectively (sd: 1.697,1.436,1.289, respectively).Finally, ADCmean and ADCmin was measured for each patient using the corresponding VOIs defined on the T2 images. Mean ADCmean value of the primary tumors was 0.834 10-3 mm2/s (sd: 0.138), while mean ADCmin value was 0.516 10-3 mm2/s (sd: 0.152) and mean lesion volume was 1.713 cm3 (sd: 1.087). Figure 2 shows the DICE indexes for each patients. Figure 3 shows two examples of concordant and discordant contouring on DICE analysis.
All imaging modalities detected the primary intraprostatic lesion, being concordant in 12/13 regarding the intraprostatic site of disease; in 1/13 patients 68Ga-PSMA PET identified the primary tumour in the left side of the prostate, while 68Ga-DOTA-RM2 PET and MRI were concordant with histology in identifying the primary tumour on the right lobe. Regarding seminal vescicle invasion (SVI), in 11/13 patients 68Ga-PSMA, 68Ga-DOTA-RM2 PET and MRI did not detect any involvement, being concordant with histology; in 2/13, histology identified SVI not seen at imaging. The validation of extracapsular extension (ECE) with histology has been performed only for MRI, as both 68Ga-PSMA and 68Ga-DOTA-RM2 PET are not suitable to identify ECE because of their limited spatial resolution. Histology and MRI were concordant in 5/13 patients (2/13 positive and 3/13 negative for ECE) and discordant in 8/13 (5/13 with ECE at histology but not on MRI and 3/13 positive on MRI but not confirmed at histology).
Discussion and conclusions
These preliminary results suggest the potential complementary role of 68Ga-PSMA PET, 68Ga-DOTA-RM2 PET and MRI in PCa characterization during the staging phase. A very innovative aspect of the present study relies on the use of PET/MRI scanner for both 68Ga-PSMA and 68Ga-DOTA-RM2, differently from the few published studies on this topic7,8. The multitracer approach offers the possibility to identify different sites of disease, thus improving disease characterization and therefore patients' management and follow-up.Acknowledgements
This research was funded by the Italian Association for Cancer Research (grant IG 2017 Id. 20571) and by the Italian Ministry of Health (PE-2016-02361273); EUDRACT number: 2018-001034-18. Signa PET/MRI system (GEMS, Wakesha, Wisconsin, USA) used in the present work has been purchased with funding from Italian Ministry of Health.References
1. Barsouk, A. et al. Epidemiology, Staging and Management of Prostate Cancer. Med. Sci. 8, 28 (2020).
2. Johnson, L. M. et al. Multiparametric MRI in prostate cancer management. Nat Rev Clin Oncol 11, 346–353 (2014).
3. de Rooij, M., Hamoen, E. H. J., Witjes, J. A., Barentsz, J. O. & Rovers, M. M. Accuracy of Magnetic Resonance Imaging for Local Staging of Prostate Cancer: A Diagnostic Meta-analysis. Eur. Urol. 70, 233–245 (2016).
4. Maurer, T., Eiber, M., Schwaiger, M. & Gschwend, J. E. Current use of PSMA-PET in prostate cancer management. Nat. Rev. Urol. 13, 226–235 (2016).
5. Mapelli, P. & Picchio, M. Initial prostate cancer diagnosis and disease staging - The role of choline-PET-CT. Nat. Rev. Urol. 12, 510–518 (2015).
6. van Kalmthout, L. W. M. et al. Prospective Validation of Gallium-68 Prostate Specific Membrane Antigen-Positron Emission Tomography/Computerized Tomography for Primary Staging of Prostate Cancer. J. Urol. 203, 537–545 (2020).
7. Fassbender, T. F. et al. Voxel-based comparison of [68Ga]Ga-RM2-PET/CT and [68Ga]Ga-PSMA-11-PET/CT with histopathology for diagnosis of primary prostate cancer. EJNMMI Res. 10, (2020).
8. Schollhammer, R. et al. 68Ga-PSMA-617 Compared With 68Ga-RM2 and 18F-FCholine PET/CT for the Initial Staging of High-Risk Prostate Cancer. Clin. Nucl. Med. 44, e535–e536 (2019).
Figures