0830
PSMA-PET vs mpMRI in prostate cancer patients with biochemical recurrence1Department of Circulation and Medical Imaging, Norwegian University of Science and Technology, Trondheim, Norway, 2Department of Nuclear Medicine and Medical Physics, St. Olavs Hospital, Trondheim University Hospital, Trondheim, Norway, 3Department of Radiology and Nuclear Medicine, St. Olavs Hospital, Trondheim University Hospital, Trondheim, Norway, 4Department of Urology, St. Olavs Hospital, Trondheim University Hospital, Trondheim, Norway, 5Department of Clinical and Molecular Medicine, Norwegian University of Science and Technology, Trondheim, Norway, 6Cancer Clinic, St. Olavs Hospital, Trondheim University Hospital, Trondheim, Norway
Synopsis
The PSMA prostate recurrence study is a multisenter prospective trial where the overall aim is to evaluate the diagnostic accuracy of 18F/68Ga-PSMA PET for detection of disease in patients with biochemical recurrence. In this preliminary analysis, we have compared the clinical imaging report of PET/CT/mpMRI to a separate evaluation of mpMRI where the radiologist was blinded to the PET results. Of 94 patients included so far, recurrent disease and/or distant metastasis was detected in 44 % (median PSA 0.4 ng/ml), according to the imaging protocol while the detection rate was 17 % for the mpMRI study scoring.
Introduction
In prostate cancer, established imaging modalities are hampered by low sensitivity for detection of disease outside the prostate. Prostate-specific membrane antgen (PSMA) PET has emerged as a promising tool and is gradually becoming part of clinical practice for staging of primary disease and recurrence. The PSMA prostate recurrence study is a prospective multicenter study directed by 180°N – Norwegian Nuclear Medicine Consortium. The overall aim of the study is to evaluate the diagnostic accuracy of PSMA PET for detection of disease in patients with biochemical recurrence, in particular with comparison to multi-parametric (mp)MRI. Here, we present a preliminary analysis of data from patients recruited from one of the participating hospitals.Methods
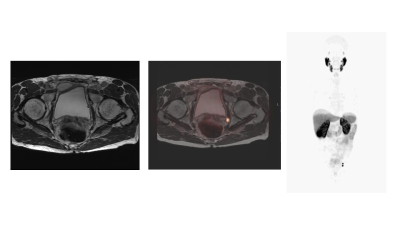
Eligible patients for this ongoing study had undergone primary radical treatment with prostatectomy or radiotherapy and presented with biochemical relapse (in accordance with the European Association of Urology) [1]. They had to be candidates for loco-regional salvage treatment. In total, 300 patients will be included from the participating hospitals. The imaging protocol of the study consists of MRI (chin to thighs), PSMA PET/CT (vertex to thighs) and PET/mpMRI of the pelvic region, performed sequentially. For 18F-PSMA-1007, PET examinations will start 120 and ~170 minutes post injection, for 68Ga-PSMA-11 examinations will start 50 and ~100 minutes post injection [1,2]. For half of the patients, PET/CT will be performed first and for the other half, PET/mpMRI first. According to the study reading protocol, the nuclear medicine physician and radiologist will evaluate and score the PET/CT, PET/mpMRI and MRI/mpMRI separately and then in consensus. An imaging report according to standard clinical practice is also compiled. In the present analysis, the imaging report based on all image modalities (PET, MRI/mpMRI, CT) according to current practice at our hospital and the MRI/mpMRI scores according to the standardized study protocol have been evaluated separately for each patient and sorted into three categories, 1) no lesions detected, 2) uncertain or 3) lesions detected. Lesions are defined as either presence of local recurrence and/or metastatic disease. Differences between groups were assessed by the Wilcoxon rank-sum test with a level of p=0.05 considered statistically significant.Results
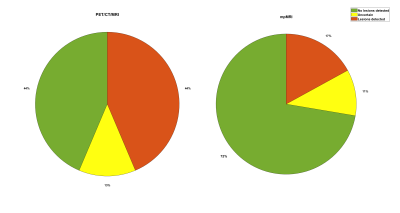
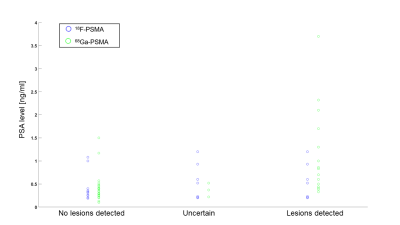
The patients in the present cohort were recruited to the study at St. Olavs hospital, between May 2020 and October 2021. Imaging reports as well as the separate MRI/mpMRI-scoring was available for 94 patients. Median patient age was 70 years (range 46-84) and median PSA level prior to imaging was 0.4 ng/ml (range 0.1-21). Based on the clinical imaging report, lesions were detected in 41, corresponding to a detection rate of 44 %. 12 patients (13%) were uncertain and for 41 (44 %) no lesions were detected. In MRI/mpMRI alone, lesions were detected in 16 patients (detection rate 17 %), while findings were uncertain in 10 (11 %) and no lesions were detected in 68 (72 %), see figure 1. For 49 patients (52 %), the score of the imaging report and the MRI/mpMRI was equal, while the imaging report score was higher than the MRI/mpMRI score for 38 patients (40 %). For seven patients (7%), the imaging report score was lower than the MRI/mpMRI score. 85 patients had previously undergone radical surgery and 9 radical radiotherapy. The median PSA level in the radiotherapy group was 4.0 ng/ml (range 0.19 – 6.80). The median PSA level in the surgery group was 0.33 ng/ml (range 0.10 – 21.0). In the surgery group, 33 patients (39 %) were examined with 18F-PSMA and 52 with 68Ga-PSMA (61 %). The detection rate was 45 % amongst patients examined with 18F-PSMA (24 % uncertain and 30 % with no lesions detected). For 68Ga-PSMA, the corresponding results were 37 %, 6 % and 58 %. The difference in distributions of the18F-PSMA and 68Ga-PSMA groups was not statistically significant (p=0.073). However, for patients with detected disease according to the imaging report, the median PSA level was lower in the 18F-PSMA than the 68Ga-PSMA group (0.38 vs 0.85 ng/ml, p=0.002).Discussion
This analysis shows a substantial increase in detection rate for recurrent prostate cancer when PSMA PET is added to MRI/mpMRI. With regards to the low median PSA of our cohort and use of both 18F- and 68Ga-PSMA, a detection rate of 44 % is comparable to other studies [5]. For 18F-PSMA-PET, there seems to be a lower PSA threshold for detection of disease than for 68Ga-PSMA, but also more cases rated as uncertain. PSMA PET most often results in an upgrading of the disease. However, several patients were downgraded when PSMA PET showed no suspicious uptake in lesions that were assessed as uncertain or malignant on MRI. Long term follow-up of the patients included in the study is necessary to evaluate the clinical concequences of adding PSMA-PET to the imaging protocol, as there is no gold standard to evaluate which lesions are true positive.Conclusion
A combined PET/CT/mpMRI imaging protocol increases the detection rate of local recurrence and metastatic disease, compared to mpMRI alone. For the complete multicenter dataset of 300 patients, we will look further into how patient management is affected by the added PET examination and whether detection rates differ between 68Ga-PSMA versus 18F-PSMA and PET/CT versus PET/mpMRI.Acknowledgements
180°N – the Norwegian Nuclear Medicine Consortium is a collaboration between the hospitals and universites in Bergen, Tromsø and Trondheim, Norway, and is supported by the Trond Mohn Foundation.
The 180°N W1 Prostate Consortium is a co-author of this abstract.
References
[1] Heidenreich A, Bastian PJ, Bellmunt J et al. EAU guidelines on prostate cancer. Part II: Treatment of advanced, relapsing, and castration-resistant prostate cancer. European urology. 2014;65(2):467-79.
[2] Giesel FL, Hadaschik B, Cardinale J et al. F-18 labelled PSMA-1007: biodistribution, radiation dosimetry and histopathological validation of tumor lesions in prostate cancer patients. European Journal of Nuclear Medicine and Molecular Imaging 2017; 44(4): 678-688.
[3] Ceci F, Oprea-Lager DE, Emmett L et al. E-PSMA: the EANM standardized reporting guidelines v1.0 for PSMA-PET. European Journal of Nuclear Medicine and Molecular Imaging 2021; 48: 1626–1638.
[4] Giesel FL, Knorr K, Spohn F et al. Detection Efficacy of 18F-PSMA-1007 PET/CT in 251 Patients with Biochemical Recurrence of Prostate Cancer After Radical Prostatectomy. Journal of Nuclear Medicine 2019; 60 (3): 362-368.
Figures