0827
1.5T Prostate MRI Utilizing Deep Learning Reconstruction in Patients with Hip Prosthesis1Radiology, Fairfax Radiological Consultants, Arlington, VA, United States, 2GE Healthcare, Boston, MA, United States, 3GE Healthcare, Lynchburg, VA, United States, 4Fairfax Radiological Consultants, Fairfax, VA, United States, 5GE Healthcare, Waukesha, WI, United States, 6GE Healthcare, Houston, TX, United States
Synopsis
While 3T offers SNR benefits for prostate imaging, patients with hip prostheses are problematic due to susceptibility artifacts and implant heating concerns. These issues are better managed at 1.5T but 1.5T lacks the SNR versus 3T. Deep learning reconstruction (DLR) may provide the SNR boost to clear this hurdle. Feasibility of 1.5T prostate MRI with DLR in patients with hip prosthesis is explored in up to 20 subjects focusing on two key contrasts in the PI-RADS guideline: T2Wand DWI. Preliminary results suggest that 1.5T with DLR might be the preferred option for patients with hip implants.
Introduction
Prostate MRl has been preferentially geared towards 3T systems due to higher SNR benefits. However, access to 3T MRI can be problematic as it is estimated that only up to 18% of MR scanners in Europe and North America are 3T while approximately 66% are 1.5T [1]. Furthermore, susceptibility artifacts and patient safety concerns at 3T pose challenges in patients who have hip implants. More than 1 million have hip implants in the USA alone [2]. There is overlap with hip arthroplasty and prostate cancer detection with average ages at 65 and 66, respectively. The number of joint arthroplasties are projected to rise rapidly [3]. Therefore, a consistent solution is needed for this patient cohort. Our hypothesis is one can synergistically combine deep learning reconstruction (DLR) and 1.5T MRI to cope with susceptibility artifacts and implant heating concerns [4] while providing adequate SNR for a PI-RADS compliant exam in a feasible scan time. We report the results of our 1.5T prostate MRI work.Methods
1.5T Signa Artist MRI equipped with AIR Recon[5] and AIR Coil (GE Healthcare, WI) was utilized for the exam. Imaging parameters meet the requirements of PI-RADS 2.1 guidelines [6]. While the image quality benefits of DLR was explored for prostate imaging [7], the previous literature is limited to T2w scans and did not explore patients with hip implants.T2W scan parameters were 18cm FOV, 2 NEX, ARC=2, 100% phase over sampling, TE=130ms, Auto TR= 5360ms, 0.4x0.7 mm in-plane resolution with 3mm slices and 0 gap. DLR SNR boost allows wider receive bandwidths of 312.5 Hz/pixel to reduce the distortion near implants while still providing diagnostic SNR as shown in Figure 1. Focus DWI technique [8] was chosen to provide better image quality than single shot DWI [9]. Focus DWI images were 18x9 cm FOV with 2.0x2.0 in-plane resolution and 3.5 mm slices with 0 gap. We collected b=50 (3 NEX) and b=800 (12 NEX) in 3:36 scan time. An ADC map was generated using b=50 and b=800 images, while the b=1400 images were synthesized via mono-exponential ADC model fitting [10]. A subset of the patients’ data were collected at both 3T and 1.5T to allow direct comparison.
Results
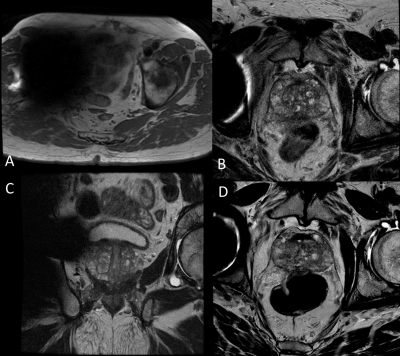
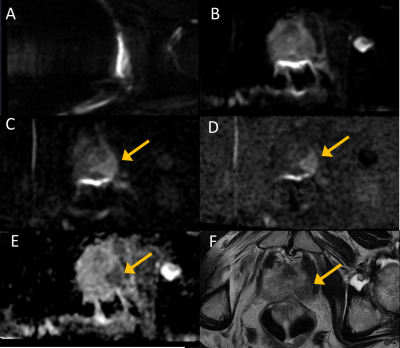
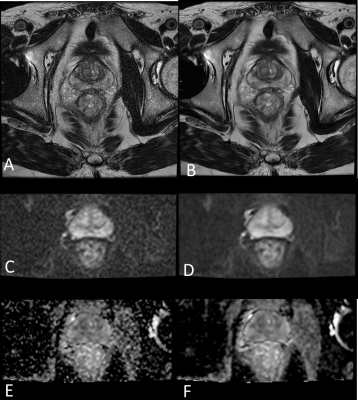
Figures 1 and 2 compare the impact of the implant on image quality between 3T versus 1.5T by scanning the same patient on both field strengths. Figure 1 compares the Axial T2W scans. As expected, 1.5T image has reduced distortion although both images have the same resolution and 312.5 Hz/pixel receive bandwidth. Scan parameters were matched between the T2W scans except for the TR which was set to Auto to provide the shortest scan time. Visually, the 1.5T image demonstrates higher SNR due to DLR versus conventional reconstruction on the 3T image.Figure 2 shows the DWI comparison at 3T versus 1.5T. 3T DWI scan was aborted after b=50 collection as signal blow out was extending beyond the prostate so only the contralateral femoral head signal remained intact. While the rectal gas related signal pile up is evident in the 1.5T DWI b=50 image, the prostate is spared from distortion from the hip prosthesis. The rest of Fig. 2 shows the DWI b=800 image, synthesized b=1400 image, the corresponding ADC map at 1.5T and matching slice location Axial T2w image highlighting the lesion. The approximately 180 mm2 tumor spans 22 mm in longest dimension, visible on the left prostatic peripheral zone with an ADC mean value of 0.855×10−3.
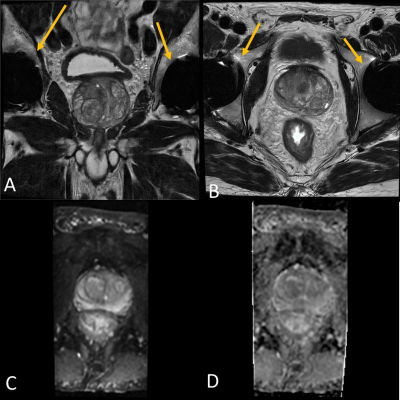
Figure 3 shows a patient with bilateral hip prostheses at 1.5T. Despite the bilateral nature of the prostheses, distortion characteristics were reasonable with high quality T2W and DWI images.
Figure 4 demonstrates the importance of protocol optimization for DWI. With Focus DWI, there is no wrap concern that it is preferential to place the readout direction anterior/posterior to minimize susceptibility artifacts due to rectal gas. In the case of distortion causing implants, placing the readout direction right/left resulted in better DWI images.
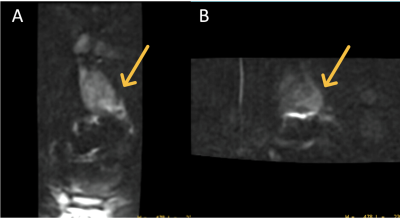
Figure 5 highlights the impact of AIR Recon DL DLR to deliver high SNR. Left column images are conventional reconstruction and right column images are the respective AIR Recon DL DLR of the same data. Both FSE T2W and DWI images show significant SNR boost, and by having higher fidelity diffusion data, ADC map quality is drastically improved. It is clear from this example that without AIRTM Recon DL, SNR is not adequate. Without DLR, the scan would be prolonged collecting more signal averages, which could result in motion artifacts or impractical exam times.
Discussion
In this work, we present the feasibility of a PI-RADS compliant 1.5T prostate imaging protocol using DLR in patients with hip prostheses. Patients imaged at both field strengths showed that 1.5T with DLR outperforms 3T in particular with prostheses that exhibit strong distortion with DWI. All 1.5T cases had good diagnostic quality in our sample cohort with a reasonable scan time of 16 minutes. One limitation of our study is the limited sample size of 20 subjects. Further data collection is warranted with different implant types, which we plan to do.Acknowledgements
No acknowledgement found.References
1. OECD. Magnetic resonance imaging (MRI) units (indicator). (2019).
2. Kremers HM, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ. Prevalence of total hip and knee replacement in the United States. The Journal of bone and joint surgery. American volume. 2015 Sep 2;97(17):1386.
3. Koff MF, Burge AJ, Koch KM, Potter HG. Imaging near orthopedic hardware. Journal of Magnetic Resonance Imaging. 2017 Jul;46(1):24-39.
4. Powell J, Papadaki A, Hand J, Hart A, McRobbie D. Numerical simulation of SAR induced around Co‐Cr‐Mo hip prostheses in situ exposed to RF fields associated with 1.5 and 3 T MRI body coils. Magnetic resonance in medicine. 2012 Sep;68(3):960-8
5. Lebel RM. Performance characterization of a novel deep learning-based MR image reconstruction pipeline. arXiv preprint arXiv:2008.06559. 2020 Aug 14.
6. Turkbey B, Rosenkrantz AB, Haider MA, Padhani AR, Villeirs G, Macura KJ, Tempany CM, Choyke PL, Cornud F, Margolis DJ, Thoeny HC. Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system version 2. European urology. 2019 Sep 1;76(3):340-51.
7. Wang X, Ma J, Bhosale P, Rovira JJ, Qayyum A, Sun J, Bayram E, Szklaruk J. Novel deep learning-based noise reduction technique for prostate magnetic resonance imaging. Abdominal Radiology. 2021 Jul;46(7):3378-86.
8. Zaharchuk G, Saritas EU, Andre JB, Chin CT, Rosenberg J, Brosnan TJ, Shankaranarayan A, Nishimura DG, Fischbein NJ. Reduced field-of-view diffusion imaging of the human spinal cord: comparison with conventional single-shot echo-planar imaging. American Journal of Neuroradiology. 2011 May 1;32(5):813-20.
9. Feng Z, Min X, Sah VK, Li L, Cai J, Deng M, Wang L. Comparison of field-of-view (FOV) optimized and constrained undistorted single shot (FOCUS) with conventional DWI for the evaluation of prostate cancer. Clinical imaging. 2015 Sep 1;39(5):851-5.
10. Cho E, Lee JH, Baek HJ, Ha JY, Ryu KH, Park SE, Moon JI, Gho SM, Wakayama T. Clinical Feasibility of Reduced Field-of-View Diffusion-Weighted Magnetic Resonance Imaging with Computed Diffusion-Weighted Imaging Technique in Breast Cancer Patients. Diagnostics. 2020 Aug;10(8):538.
Figures