0824
Radiological Evaluation of Model-Based Reconstruction for Through-Plane Resolution Enhancement in T2-Weighted Spin-Echo Prostate MRI
Eric A. Borisch1, Adam T. Froemming1, Roger C. Grimm1, Akira Kawashima2, Joshua D. Trzasko1, and Stephen J. Riederer1
1Radiology, Mayo Clinic, Rochester, MN, United States, 2Radiology, Mayo Clinic, Phoenix, AZ, United States
1Radiology, Mayo Clinic, Rochester, MN, United States, 2Radiology, Mayo Clinic, Phoenix, AZ, United States
Synopsis
Results of a radiological review of a previously described Model Based Iterative Reconstruction (MBIR) compensating for slice profile arising in a thick and overlapping-slice acquisition of the prostate are detailed. Blinded review by two radiologists indicated improvements in SNR, contrast fidelity, and diagnostic quality.
Introduction
T2-weighted spin-echo (T2SE) imaging acquires slices which are much thicker (3mm) than the typical inplane resolution (0.5-0.7mm). To address this, investigators are developing means to generate thinner slices from thick-slice data1. However, associated with thinner slices is loss of SNR. A model-based iterative reconstruction (MBIR) has been described2 for solving the through-plane resolution enhancement problem posed by a stack of 2D acquisitions acquired with overlapped slices which provides some SNR retention. In this work, we present the results of a radiological review of MBIR when applied to prostate MRI.Methods
All human studies were performed using a protocol approved by the IRB, and all subjects provided written consent. Subjects for whom an MRI exam was clinically indicated were recruited and imaged using a T2SE sequence in axial orientation using the parameters: TR 3000, TEEFF 100 msec; ETL 21, FOV 20 cm, R=1.5 acceleration, 0.62 × 0.71 mm2 inplane resolution, 90 overlapping slices each 3mm thick with 1mm slice-to-slice increment, scan time 6:40. Glucagon or a similar motion-suppressant was not used. For each exam the data were subjected to the standard linear reconstruction1 and MBIR, each providing axial slices with nominal 1mm thickness. The MBIR algorithm has a regularization parameter λ which controls the tradeoff of SNR retention vs. resolution loss, the latter also manifest as “blotchy” contrast. In six initial calibration subjects MBIR results were generated for the range λ = 0.0001 to 0.0008. Two uroradiologist reviewers selected by consensus λ = 0.00015 as the value providing the best compromise of SNR retention with resolution, and that value was used for the subsequent comparison. Next, 16 subjects were imaged using the described T2SE sequence, and linear- and MBIR-reconstructed stacks of 1mm thick images were generated. For each subject the two resultant image series were presented to the reviewers in random order (Series A, B) with identifying information removed.The two series were compared (A vs. B) using multiple criteria. These were: relative SNR, contrast, fidelity of contrast (lack of patchiness or blur), and other artifact. They were also compared for sharpness of: prostate capsule, interface between transition (TZ) and peripheral zone (PZ), seminal vesicles, any structures within TZ or PZ. Comparisons were done using a five-point scale (-2: Series A markedly superior to Series B; -1: Series A superior to Series B; 0: Series A equivalent to Series B; +1: Series A inferior to Series B; +2: Series A markedly inferior to Series B). Finally, each series was evaluated individually for overall diagnostic quality (0: non-diagnostic, 1: adequate for diagnosis; 2: more than adequate for diagnosis).
Results
Figure 1 shows images from one of the calibration studies, illustrating dependence of image appearance on parameter λ. Figure 2 shows results from the radiological evaluation. As shown, for metrics having a statistically significant difference in preference (7/10), the MBIR reconstruction was preferred. For two metrics, SNR (Fig. 2A) and fidelity of contrast (lack of patchiness, smudginess, or blur, Fig. 2H), this was pronounced (p < 0.001). Overall diagnostic quality scores (Fig. 2J) show preference for MBIR. Non-diagnostic scores were principally due to motion effects.Figure 3 shows linear (A) and MBIR (B) images from Subject #4, with MBIR rated by both reviewers as having superior SNR and sharpness of PZ structures vs. linear reconstruction. Also shown are images from linear (C) and MBIR (D) from Subject #8, with MBIR rated by both reviewers as having provided more than adequate overall diagnostic quality vs. adequate quality for linear.
Conclusion
MBIR provides a significant improvement in SNR, contrast, and sharpness of structures in the PZ and TZ vs. linear reconstruction in high through-plane resolution (1mm thick) T2SE images of the prostate. There was no diminished performance for any of the other evaluation criteria.Acknowledgements
No acknowledgement found.References
- Kargar S, et al. Modified acquisition strategy for reduced motion artifact in super resolution T2 FSE multislice MRI: Application to prostate. MRM 2020;84(5):2537-2550
- Borisch E, et al. Iterative Reconstruction for Enhanced Through-Plane Resolution T2-Weighted Spin-Echo Imaging of the Prostate. ISMRM 2021; 1185
Figures
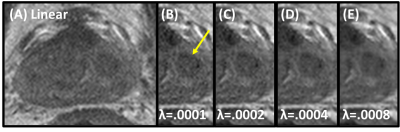
Image from linear reconstruction (A) and from MBIR (B-E) showing impact of regularization value. Nodule (B, arrow) shows increased objectionable patchy contrast with increasing regularization.

Radiologist relative preferences comparing linear to MBIR reconstructions. Wilcoxon signed rank significances of < 0.05, 0.01, and 0.001 flagged with *, **, and ***, respectively.
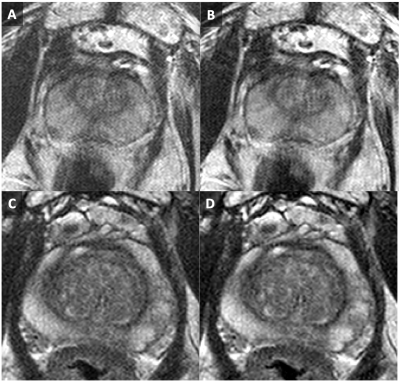
Comparison of Linear (A, C) vs. MBIR (B, D) from two different patient studies. See text for additional details.
DOI: https://doi.org/10.58530/2022/0824