0822
Role of puborectalis thickness measurement in the assessment of pelvic floor dysfunction and its correlation with HMO classification.1Radiology, Loyola University Medical Center, Maywood, IL, United States, 2Biostatistics, Oakland University, Rochester, MI, United States, 3Radiology Body MRI, Stanford University Medical Center, Palo Alto, CA, United States
Synopsis
Pelvic floor dysfunction is a common problem affecting women over 50 years of life causing significant morbidity. Traditionally, H-line and M-line measurements have been used to assess pelvic organ prolapse. However, puborectalis muscle which plays a crucial role in pelvic floor intactness can be measured to reflect the weakening of the pelvic floor. We evaluated and found puborecatalis measurement can be used as a supplement to H-line and M-line measurements in assessing pelvic organ prolapse.
Introduction
Pelvic floor dysfunction affects about half of women over the age of 50 years and causes significant morbidity. MR defecography compliments the clinical examination which was once the primary method of evaluating pelvic floor dysfunction. The puborectalis muscle is one of the three important components of the levator ani muscles, which are crucial for maintaining the intactness of the pelvic floor. Thinning of puborectalis muscle and tears in the muscle can result in pelvic organ prolapse/ herniation of pelvic viscera. MR defecography examinations for evaluating pelvic floor dysfunction primarily depend on H-line and M-line measurements for diagnosing pelvic organ prolapse. Abnormal H-line and M- line measurements reflect the widening of the pelvic floor and subsequent pelvic organ prolapse. Puborectalis thinning or defect can result in weakening of pelvic floor and be reflected upon by abnormal H-line and M-line measurements. Hence, puborectalis thickness (PT) are simple and quick adjunct measurements with much less interobserver variability in the measurement techniques in the MR defecography examinations.The objective of our study was to correlate PT measurement to the LHW, H-line and M-line in the presence of pelvic organ prolapse.
Methods
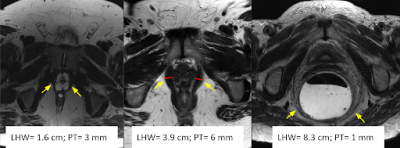
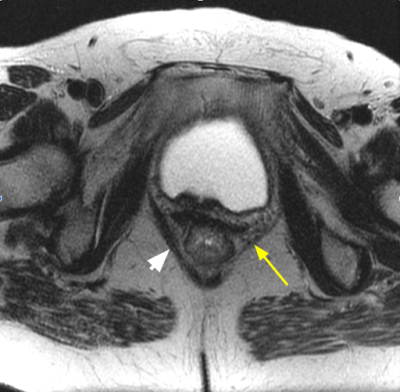
A retrospective review of 70 consecutive MR defecography examinations performed on 3T MRI scanners in a single institution over a period of 2 months (June 2019- August 2019). All symptomatic females above 18 years of age referred for concern of pelvic floor dysfunction were included in the study. As part of the MR defecography examination, axial T2 weighted images of the pelvis were obtained as axial to body plane (4 mm slice thickness, TR 800, TE 150, FOV 24 cm, 512 x 256 matrix). Based on the literature review, the PT is measured on the resting phase axial T2 sequence at the inferior margin of the pubic symphysis. It is the diameter between the inner and outer margins of the puborectalis sling at its maximum muscle bulk, and similarly the contralateral sling measurement was also recorded to assess symmetry of the muscle. In asymmetric muscle thickness, the smaller of the muscle slings were chosen for measurement. The images were reviewed, and the following was documented for analysis: age, clinical indication, PT, H-line, M-line, anorectal angle (ARA) measurements in resting, during Kegel maneuver and dynamic defecation. Based on the measurements, the anterior, middle, and posterior compartment pelvic floor descent was graded and compared with PT measurements. Statistical analysis was performed using one-way ANOVA, Fisher’s exact test, chi-square test and descriptive statistics.Results
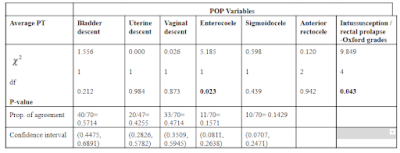
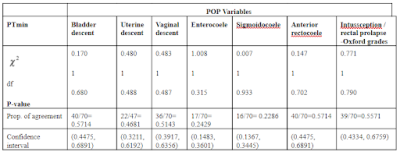
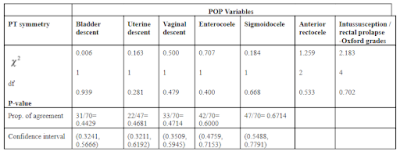
We had 70 female patients between the ages of 23 and 90 years, of which 27 patients had a hysterectomy. The mean PT measured at the level of LHW was 5.5 mm, and SD was 2.5 mm, with the lowest thickness of 1.7 mm and the highest PT 11.5 mm. Asymmetric PT was present in 6 patients (12%) and focal defect in the puborectalis muscle in 2 patients (4%). The LDW was abnormal in 19 patients (38%) with the smallest LHW being 2.2 cm and the widest LDW 7.2 cm. The mean LDW was 4.4 cm and the standard deviation (SD) was 1.1 cm. Chi-square test of independence between average PT and various pelvic organ prolapse (POP) showed there was statistically significant association between average PT and enterocoele (p=0.02), and rectal intussusception (p=0.04). (Table 1) On the contrary, when the minimum PT was analyzed, there was no statistically significant correlation with the POP. (Table 2) We found that there was negative correlation between LHW and minimum PT which proves that when there is reduced thickness of puborectalis muscle, there is increased width of levator hiatus which predisposes to the pelvic organ prolapse. We found that presence or absence of symmetry in the puborectalis thickness also has no relation to the different POP. (Table 3)Discussion
Literature review mentions different puborectalis muscle thickness thresholds measured on the axial MR sequences. However, there are no large studies and uniformity in the measurement techniques prescribed by various authors, and also most of these studies were performed on nulliparous asymptomatic women. Though these serve as a good reference in nulliparous women, this may not be applicable in the common age group of patients who usually present to the urogynecology clinics with pelvic organ prolapse symptoms. 38% of patients in our sample had a hysterectomy which could be a risk factor for pelvic floor weakness. In our study with symptomatic patients, we found that the normal PT was > 5.1 mm + 2.5 mm. The asymmetry of the puborectalis muscle slings more than 2.5 mm of the contralateral side may represent a weakness of muscle which can predispose to avulsion and/ or pelvic organ prolapse. Limitation of our study was small sample size of 70 patients. Future large cohort studies to correlate the asymmetry of puborectalis with a clinical history of obesity, constipation or complicated or prolonged second stage of labor would be beneficial.Conclusion
Puborectalis thickness <5 mm can be used as a cut-off for determining patients at risk for pelvic organ prolapse, especially those with asymmetric thinning or puborectalis defect.Acknowledgements
NoneReferences
1. Dietz HP, Severino M, Atan IK, Shek KL, Rojas RG. Warping of the levator hiatus: how significant is it? Ultrasound Obstet Gynecol 2016;48:239-242.
2. Gregory WT, Nardos R, Worstell T, Thurmond A. Measuring the levator hiatus with axial MRI sequences: Adjusting the angle of acquisition. Neurourology and Urodynamics 2011;30:113-116.
3. Colaiacomo MC, Masselli G, Polettini E, Lanciotti S, Casciani E, Bertini L, Gualdi G. Dynamic MR Imaging of the pelvic floor: a pictorial review. Radiographics 2009;29:3,e35.
4. del Salto LG, Criado JM, Velasco lG, et al. MR Imaging-based assessment of the female pelvic floor. Radiographics 2014;34:1417-1439.
5. Margulies RU, Hsu Y, Kearney R, Stein T, Umek WH, DeLancey JOL. Appearance of the levator ani muscle subdivisions in magnetic resonance images. Obstet Gynecol. 2006; 107(5):1064-1069.
Figures