0821
Assessment of pessary position using upright MR imaging of patients with pelvic organ prolapse1Magnetic Detection & Imaging, University of Twente, Enschede, Netherlands, 2Multi-Modality Medical Imaging, University of Twente, Enschede, Netherlands
Synopsis
Pessary treatment for pelvic organ prolapse (POP) has a success rate of only 63% and its working mechanism remains unclear. This study applies upright MRI to gain insight into pessary. Patients were scanned in supine and upright position. The pessary was located under the inferior pubic bone in 7 out of 9 patients in upright position, opposed to 1 out of 9 in supine position. This indicates that the pubic bone does not (solely) contribute to the supporting mechanism. The use of upright MRI contributes to knowledge about the working mechanism of the pessary.
Introduction
Pelvic organ prolapse (POP) is a common condition in elderly women, with a prevalence of 11% between the ages of 45-85 years in the Netherlands1. A pessary is a relatively simple and cheap device to treat POP. However, the success rate after 3 months is only 63%2. Successfactors on pessary fitting are described, but are mainly based on global physical factors (e.g. previous hysterectomy, overweight, hiatal circumferences). A universally accepted view on the working mechanism of a pessary, including support tissue, is lacking. This is most easily proved by the variation in the position and effect of a pessary protrayed in scientific papers and patient information folders. Little research has been done to better understand the actual position of the pessary and the location of the prolapsed organs before and after pessary insertion. Since physical examination, typically done in supine position, is unable to present us with a 3D multicompartment view, imaging is needed.Magnetic Resonance Imaging (MRI) allows for multicompartment pelvic imaging. There are currently a few low-field MRI scanners available that provide the opportunity to scan patients in different body positions3,4. Since the amount of prolapse in upright position is significantly larger than in supine position5, this technique is crucial for a realistic evaluation of the working mechanism of a pessary.
This research aims to determine the position and orientation of the pessary in patients with POP in upright position and compare this to the position and orientation in supine position, to obtain a better understanding of its working mechanism.
Methods
In this study in total 15 patients wearing their ring shaped pessary for at least three months will be scanned in upright and supine position using a 0.25T MRI scanner (Esaote SpA, Genoa, Italy). Until now, 9 patients were scanned, all between 16:00 and 18:004, and emptied their bladder 15 minutes before the scan. A multi-slice T2-weighted fast spin echo was acquired in the sagittal plane, using the following parameters: TE/TR: 25/3480 ms, flip angle 90°, reconstructed resolution: 1.3×1.3 mm2, slice thickness: 5 mm, number of slices: 11, total scan time: ≈2 min.On the acquired scans the distance between the most inferior part of the pessary and the Pelvic Inclination Correction System (PICS) reference line6 was measured (dpess) and compared between upright and supine position using the Wilcoxon signed-rank test. Furthermore, the angle between the pessary and the PICS (αpess) was measured and compared between upright and supine position.
Results
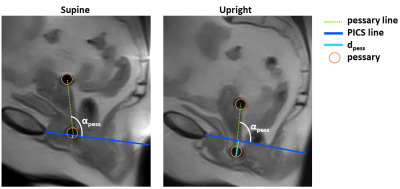
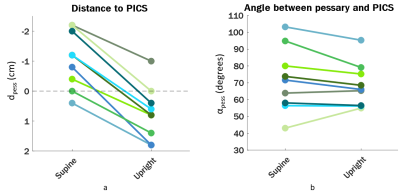
As can be seen in Figure 1, the pessary can be clearly seen on the MR image. The figure also shows an overview of the drawn lines and calculated variables. The PICS line originates at the inferior pubic point and descends from there in 8 out of 9 patients. This means that when the pessary is located lower than the PICS line, the pessary is also located lower than the inferior pubic point.Figure 2a shows an overview of dpess of al patients in supine and upright position. It can be seen that in upright position the pessary is located lower in all patients, with a median (min, max) descent of 1.8 (1.2, 2.6) cm (p = 0.008). The lowest point of the pessary is located lower than the PICS line in 1 out of 9 patients in supine position, and in 7 out of 9 patients in upright position. As can be seen in Figure 2B, there is only a slight change in αpess between supine and upright position, varying from increase to decrease. The median (min, max) difference between upright and supine is -5 (-16, 1) degrees (p = 0.16).
Discussion
The difference in αpess between supine and upright position is small, but there is a significant descent of the pessary observed in all patients in upright position. Furthermore, the lowest point of the pessary is located lower than the inferior pubic point in 7 out of 9 patients, indicating that there has to be at least an additional support mechanism of the pessary than solely the pubic bone, as was hypothesized before7. This phenomenon can only be observed when patients are in the upright position, indicating that imaging in this position is of importance for further evaluation of the working mechanism of the pessary in patients with POP.This research was performed using 2D sagittal images on which the PICS and the pessary angle were used as parameters to analyze the pessary position. 3D analysis would enable research into additional parameters that may be useful to investigate the working mechanism of the pessary, such as the position and orientation in the coronal and transverse plane and the relationship between the pessary position with reference to the pelvic organs.
Conclusion
This research showed a descent of the pessary in upright body position compared to supine, and the difference in position relative to the PICS line and inferior pubic point. A pessary position lower than the inferior pubic point indicates that the pubic bone does not (solely) contribute to the support of the pessary. Upright MRI gives more insight into the working mechanism of a pessary in patients with POP in its most relevant body position.Acknowledgements
No acknowledgement found.References
1. Slieker-ten Hove MCP, Pool-Goudzwaard AL, Eijkemans MJC, Steegers-Theunissen RPM, Burger CW, Vierhout ME. Symptomatic pelvic organ prolapse and possible risk factors in a general population. Am J Obstet Gynecol. 2009; 200(2):184.e1-184.e7.
2. Manzini C, Morsinkhof LM, van der Vaart CH et al. Parameters associated with unsuccessful pessary fitting for pelvic organ prolapse up to three months follow-up: a systematic review and meta-analysis. Int Uroynecol J 2021 (in press).
3. Williams HG, Cooper A, Hodgen L at al. Upright pelvimetry using MRI for the prediction of birth associated cephalo-pelvic disproportion following induction of labour. Proc Intl Soc Mag Reson Med 28 (2020); submission 2571
4. Morsinkhof LM, Grob ATM, Veenstra van Nieuwenhoven AL, Simonis FFJ, Upright MR imaging of daily variations in pelvic organ position for assessment of pelvic organ prolapse. Proc Intl Soc Mag Reson Med 29 (2021); submission 3691
5. Grob ATM, Heuvel J olde, Futterer JJ, et al. Underestimation of pelvic organ prolapse in the supine straining position, based on magnetic resonance imaging findings. Int Urogynecol J 2019;30(11):1939-1944.
6. Betschart C, Chen L, Ashton-Miller JA, DeLancey JOL. On pelvic reference lines and the MR evaluation of genital prolapse: A proposal for standardization using the Pelvic inclination correction system. Int Urogynecol J. 2013; 24(9):1421-1428.
7. Hong CX, Meer E, Cioban M et al. Position and orientation of vaginal pessaries in situ on magnetic resonance imaging. Int Urogynecol J. 2021.
Figures