0808
Inline Implementation of Motion-Compensated, High-Resolution Myocardial Perfusion Imaging: Initial Experience1MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom, 2Evelina London Children’s Hospital, Guy’s and St Thomas’ NHS Foundation Trust, London, United Kingdom, 3Biomedical Engineering and Imaging Science, King's College London, London, United Kingdom
Synopsis
This abstract describes a feasibility study for a high-resolution perfusion imaging framework, including a dedicated sampling pattern and a motion compensation framework integrated into temporal regularization and implemented in-line on the scanner with GPU support. The approach was employed successfully in patients with suspected myocarditis at rest, showing superior ability to handle both respiratory and cardiac motion at an image resolution of 1.3 mm2, as compared to a clinical reference perfusion sequence and supported by Late Gadolinium Enhancement imaging findings.
Introduction
Standard clinical myocardial perfusion MR techniques are hampered by a lack of spatial resolution and coverage. Both cardiac and respiratory motion are a challenge to image quality, and necessitate breath held exams and very fast single-shot acquisitions, with acquisition duration of single slices being the limiting factor for anatomical coverage. To increase spatial resolution and/or shorten single-shot acquisition times, high acceleration factors are usually unavoidable. These are, however, only achievable with some degree of regularization along the temporal dimension of the dynamic perfusion series, which leads to strong blurring artifacts in the case of motion between frames. This abstract describes a feasibility study for a high-resolution perfusion imaging framework, including a dedicated sampling pattern and a reconstruction which incorporates motion compensation in the temporal regularization implemented in-line on the scanner with GPU support.Methods
An MR perfusion prototype sequence for a 2D single-shot, saturation-recovery acquisition was implemented featuring a dedicated sampling pattern combining incoherent undersampling for high-, and linear undersampling low spatial frequencies. A prototype reconstruction with motion compensation was implemented inline on the scanner with GPU support, featuring a preliminary reconstruction of all frames at reduced resolution without temporal regularization, an estimation of non-rigid motion fields between all frames1, and a final reconstruction with incorporation of motion fields into a temporal regularization term2,3. The described sequence and reconstruction were applied in 3 patients with suspected Myocarditis (ages 12, 16 and 17 years) on a 3T Scanner (MAGNETOM Vida, Siemens Healthcare, Erlangen, Germany), with the following parameters: 1.3mm2 acquired resolution, 8 mm slice thickness, 3-4 slices per heartbeat, acceleration factor 5.5-6.0, FLASH readout, TE/TR 1.19/2.71 ms, BW 707 Hz/px, TI 110 ms, FA 15 deg, chemical-shift selective fat saturation, single slice readout time 105 ms (excluding sat pulses, delay times and FatSat). The sequence was applied for 90 dynamics in free breathing during a bolus injection (0.15 mmol/kg Gadobutrol), and reconstructed with (MC) and without (NMC) the integrated motion compensation. In addition, a standard clinical sequence was applied as a reference directly afterwards for 40 dynamics (acquired/reconstructed resolution 2.3 x 1.9 / 1.9 x 1.9 mm2, TPAT acceleration factor 2, TE/TR 1.03/2.16 ms, BW 1003 Hz/px, TI 95 ms, single slice readout time 125 ms).Results
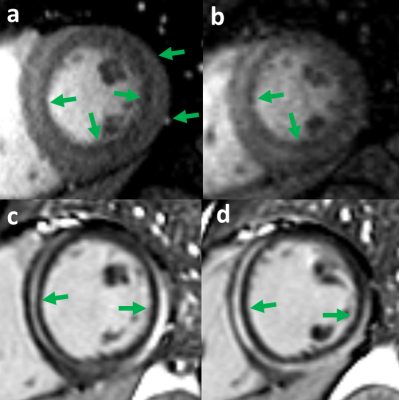
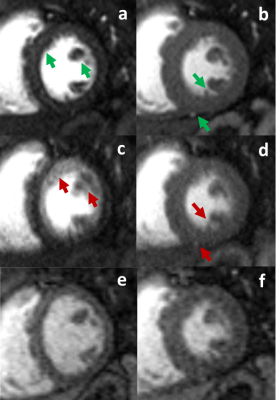
In-line image reconstruction times for the described high-resolution sequence were 20-30 s per slice. Image quality for MC was excellent in all cases despite heavy respiratory and cardiac motion as revealed by the comparison of MC and NMC reconstructions. Figure 1 shows a comparison of MC and NMC images in a patient at different points during the perfusion series. For the same patient, Figure 2 shows MC, TPAT and LGE images, the latter confirming acute myocarditis and validating the contrast pattern seen in both MC and TPAT images during the last frames. Figure 3 shows a second patient with both cardiac and respiratory motion, leading to significant blurring in NMC, but no significant degradation in MC images.Discussion
Despite the limited amount of clinical data, the study at hand demonstrates feasibility for a fast in-line implementation of free-breathing, high-resolution myocardial perfusion data in a clinical setting. While further validation studies are warranted to demonstrate the added clinical value of the presented approach, cases shown here, including confirmation by LGE findings, hint at the potential for superior depiction of small perfusion abnormalities.Conclusion
A high-resolution, free-breathing myocardial perfusion approach with a fast, inline motion-compensated reconstruction was employed successfully in patients with suspected myocarditis, showing very good ability to handle both respiratory and cardiac motion at a resolution of 1.3mm2.Acknowledgements
No acknowledgement found.References
1) Xue H, Zuehlsdorff S, Kellman P, et al. Unsupervised inline analysis of cardiac perfusion MRI. In Proceedings of the International Conference on Medical Image Computing and Computer-Assisted Intervention, 2009, 741-749.
2) McElroy S, Kunze KP, Nazir S, et al. Stress first pass myocardial perfusion using simultaneous multi-slice (SMS) SSFP with iterative reconstruction and integrated motion compensation. Proceedings of the Annual SCMR Meeting, 2021.
3) Muehlberg F, Stoetzner A, Forman C, et al. Comparability of compressed sensing-based gradient echo perfusion sequence SPARSE and conventional gradient echo sequence in assessment of myocardial ischemia. European Journal of Radiology, 2020, 131:109213.
Figures