0791
Effects of Respiration on Aortic Pulse Wave Velocity using Retrospective Respiratory Gated Radial 2D Phase Contrast MRI1Dept of Medical Physics, University of Wisconsin - Madison, Madison, WI, United States, 2Dept of Medicine, University of Wisconsin - Madison, Madison, WI, United States, 3Dept of Radiology, University of Wisconsin - Madison, Madison, WI, United States
Synopsis
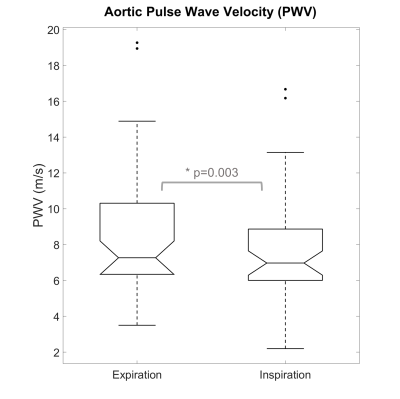
Pulse wave velocity (PWV) is a non-invasive biomarker related to vascular stiffness and cardiovascular risk. Cine 2D phase contrast (2DPC) MRI can be used to assess aortic PWV. However, the effects of respiration on PWV measures remain unexplored. Here, we assessed the effects of respiration by retrospectively gating free breathing radially sampled 2DPC MRI data in both inspiration and expiration. Two axial slices were obtained in the aortic arch and abdominal aorta and time shift methods were used to calculate PWV between the ascending and abdominal aorta. PWV measurements from inspiration (7.58m/s) were significantly decreased relative to expiration (8.42m/s).
Introduction
Pulse wave velocity (PWV) is the velocity of blood pressure pulsations through arterial vasculature and is inversely related to arterial compliance via the Moens-Korteweg equation1. Cine 2D phase-contrast (2DPC) MRI has been successfully used to non-invasively determine aortic PWV by measuring temporal shifts in flow waveforms between imaging planes and calculating the aortic centerline distances between planes2. Typically, these 2DPC exams are performed under breath-hold conditions at end-expiration. However, pressure tonometry studies have shown that carotid-radial PWV measures obtained during peak inspiration are decreased relative to expiration3, an effect that has not been demonstrated using MRI. Recently, free-breathing methods using radially sampled 2DPC MRI have been introduced for aorta PWV measurements for patients unable to hold their breath or follow commands in the bore and to increase patent comfort. Coupled with retrospective respiratory and cardiac gating4,5, such continuous radial acquisitions enable flexibility in the reconstruction of cine PC series to user-selected respiratory phases. Here, we utilize free-breathing radial 2DPC MRI to retrospectively reconstruct data during both inspiration and expiration to measure their effects on MRI-derived aortic PWV measurements.Methods
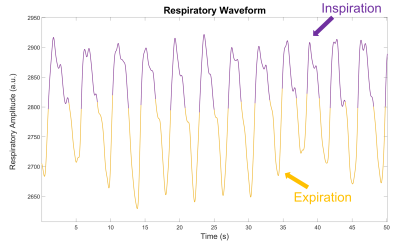
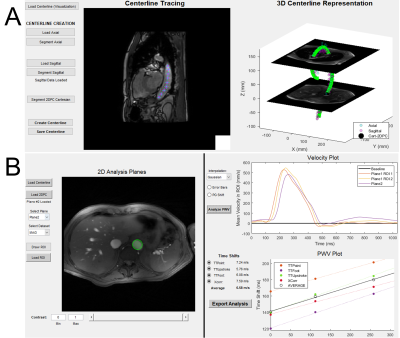
Forty-five healthy subjects (35F/10M, mean age=64y) were analyzed from a cohort of late-middle-aged subjects enriched with risk for late-onset Alzheimer’s disease. Free-breathing radial 2DPC MRI chest scans were performed at 3T (Discovery MR750, GE Healthcare, WI) using an 8-channel chest coil. Two axial planes were placed in the aorta: one in the aortic arch and the second in the abdominal aorta (Figure 1). Cine 2DPC scans were acquired with: peripheral pulse oximeter gating (PPG); TR/TE=7.5/4.3ms; flip=25˚; # radial projections=10,032; slice thickness=6mm; VENC=150cm/s; reconstructed cine cardiac frames=40; non-interpolated mean temporal res.=25.2ms; scan time=2.5min. Additionally, ungated, Cartesian, free-breathing anatomical FIESTA images (sagittal, coronal, and axial) were acquired to semi-automatically trace centerlines for distance calculations. Respiratory gating signals were acquired with a respiratory belt. Two separate cine reconstructions of the radial data were performed with a 50% acceptance window that continuously adapted to (1) expiration and (2) inspiration positions, as shown in Figure 2. PPG and respiratory gating signal quality was assessed for each subject and for each imaging slice.A customized user-interface (available on Github) was developed in MATLAB (Mathworks, MA) to calculate centerlines and process 2DPC data to computed PWV. 3D b-spline centerlines were traced from the anatomical FIESTA images by manually placing points in the aorta over all image slices where the aorta was visualized. Centerlines distances were kept constant for inspiration and expiration. From the first 2DPC plane in the aortic arch, both ascending and descending aorta were transected thus providing two ROI data measurements. Circular ROIs were drawn around each vessel and flow waveforms were constructed over all time frames. Obtained flow waveforms were smoothed with a Gaussian filter (width 7 pixels) and linearly interpolated (20x). Cross correlation (Xcorr)6 methods were used to calculate time shifts in flow waveforms. Measured time shifts were plotted against measured centerline distances between planes and linear regression was used to fit the 3 data points, where the inverse of the fitted slope is the estimated global aortic PWV (Figure 2B). Two-tailed paired t-tests were performed to assess differences between PWV values obtained from inspiration and expiration.
Results
Inspiration- and expiration-gated 2DPC data were successfully obtained in 44 subjects. One subject was excluded due to poor respiratory gating signal. After statistical analysis, global aortic PWV values reconstructed during inspiration (mean=7.58, SD=2.91 m/s) were significantly lower (p=0.003, CI=[-1.25,-0.278]) compared to PWV values reconstructed during expiration (mean=8.42, SD=3.38 m/s). Box plots for inspiration and expiration data are shown in Figure 4.Discussion
This study demonstrated a significant decrease (9.9%) in aortic PWV measurements obtained with 2DPC MRI during inspiration versus expiration. These results are consistent with findings from a pressure tonometry study evaluating carotid-radial PWV under deep, prolonged inspiration and expiration, where they also found a decrease between expiration and inspiration3. However, in our study, subjects underwent normal respiration, which may show different effects relative to deep, sustained respiration. The physiological mechanisms for this are unclear, however, it is known that respiration acts on (1) intrathoracic pressure, (2) atrial filling and cardiac output, (3) arterial pressure, (4) arterial baroreceptors, and (5) blood flow rates. Additionally, sustained breath-holds induce additional pressure changes and may create short-term hypoxic conditions that affect vascular tone and vessel dilation7. These findings have an important implication for both 2DPC PWV studies, which are typically performed under breath-hold conditions, and for free-breathing 2DPC and 4D flow MRI PWV studies, which are typically gated on expiration.Conclusion
We found that aortic PWV measurements obtained during inspiration were around 10% lower than expiration using retrospectively gated, free-breathing, radial phase contrast MRI. Future studies look to increase sample size, validate these findings with breath-hold 2DPC exams in both sustained inspiration and expiration, and evaluate volumetric flow rates and area changes in both respiratory phases.Acknowledgements
We gratefully acknowledge research support from GE Healthcare and funding support from the National Institutes of Health (F31- AG071183, KL2-TR002374, R01-AG027161, R01-AG062167).References
1. Callaghan FJ, Geddes LA, Babbs CF, Bourland JD. Relationship between pulse-wave velocity and arterial elasticity. Med Biol Eng Comput 1986;24(3):248-254.
2. Wentland AL, Grist TM, Wieben O. Review of MRI-based measurements of pulse wave velocity: a biomarker of arterial stiffness. Cardiovasc Diagn Ther 2014;4(2):193-206.
3. Murphy J, Manoharan G, Adgey A. EFFECT OF RESPIRATION ON PULSE WAVE VELOCITY MEASUREMENTS IN THE ARM: PP.8.314. Journal of Hypertension 2010;28:e144.
4. Roberts GS, Johnson KM, Kecskemeti S, et al. Feasibility of a Free-Breathing 2D Phase Contrast MRI for Aortic Pulse Wave Velocity Measurements. ISMRM; 2020. p. 89.
5. Schrauben EM, Anderson AG, Johnson KM, Wieben O. Respiratory-induced venous blood flow effects using flexible retrospective double-gating. J Magn Reson Imaging 2015;42(1):211-216.
6. Fielden SW, Fornwalt BK, Jerosch-Herold M, Eisner RL, Stillman AE, Oshinski JN. A new method for the determination of aortic pulse wave velocity using cross-correlation on 2D PCMR velocity data. J Magn Reson Imaging 2008;27(6):1382-1387.
7. Sobol KV, Burdygin AI,
Nesterov VP. The Effect of Short-Term Breath Holding on Pulse Wave Velocity and
Vascular Stiffness. Biophysics 2019;64(6):978-983.
Figures