0764
Intravoxel incoherent motion (IVIM) MRI for juvenile idiopathic arthritis in the knee: a prospective pilot study1Department of Internal Medicine II, Ulm University Medical Center, Ulm, Germany, 2Department for Diagnostic and Interventional Radiology, Ulm University Medical Center, Ulm, Germany
Synopsis
Intravoxel incoherent motion (IVIM) imaging allows the quantification of diffusion and pseudo-perfusion in tissues and has been proposed as an alternative to conventional contrast agent enhanced (CE) T1-weighted scans. Its qualitative benefits for diagnosing juvenile idiopathic arthritis in the knee has previously been demonstrated. In this work, quantitative data of diffusion and perfusion fraction values between synovitis patients and healthy volunteers were compared in a prospective setting.
Introduction
Diffusion-weighted imaging (DWI) is a widely applied quantitative MRI method for the detection of diffusion of water molecules in tissues, however, the calculation of the apparent diffusion coefficient (ADC) with a single-exponential model does not reflect the impact of microperfusion effects on the ADC [1]. Intravoxel incoherent motion (IVIM) imaging extents the conventional ADC model by additional consideration of the micro-vessel perfusion in tissues from multi-b-value DWI scans [2].Patients with juvenile idiopathic arthritis (JIA), one of the most common entities of chronic arthritis in children and adolescents, are usually examined by use of T1-weighted MR scans with intravenous application of gadolinium-based contrast material for the visualization of inflamed synovial tissue and to assess disease activity and response to therapy. Previous work has shown that perfusion fractions calculated with IVIM MRI improves diagnostic performance and confidence by allowing the visual differentiation of joint effusion and inflamed synovium without the use of contrast agents [3].
In this work quantitative data of diffusion and perfusion fraction values between synovitis patients and healthy volunteers were compared in a prospective setting.
Methods
In this study, 9 patients with 11 symptomatic knee joints (mean age: 13 +/- 6 years) with known or suspected arthritis of the knee and 5 healthy volunteers with 10 knee joints (mean age: 27 +/- 4 years) were included. Written informed consent was obtained in all cases. All data were acquired on a 3T whole-body MRI (Skyra, Siemens Medical, Germany) with a dedicated 15-channel transmit/receive knee coil. Patients and volunteers underwent an examination including a survey scan and a readout-segmented multi-shot EPI(RESOLVE) DWI scan with 10 B-values: 0, 50, 100, 150, 200, 300, 400, 600, 800 and 1000 mm/s2. Further scan parameters were TR/TE=3400/57ms, resolution of 1.3 x 1.3 x 3 mm, 14 slices, FOV of 180 x 180 mm and a scan duration of 5:32min. Additionally, post-contrast transverse T1-weighted turbo spin echo (CE-T1w) was acquired from the patients. Fitting of the diffusion D, perfusion/pseudo-diffusion D* and perfusion fraction f parameter maps, was performed using a bi-exponential fitting model: $$S = S_{0}((1-f)e^{-bD}+fe^{-bD^{*}})$$with the measured signal intensity without diffusion-weighting (b=0) used as $$$S_{0}$$$.
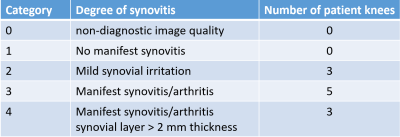
Quantitative analysis of the data was performed by manually drawing three ROIs in muscle, synovial membrane and effusion for each data set from which the mean diffusion coefficient and perfusion fraction was calculated. Two board-certified pediatric radiologists independently completed all qualitative image analysis for the patient group. Presence and degree of synovitis were recorded by each reader on a modified 5-item Likert scale (see also table 1). The categories 3 and 4 were considered to represent manifest synovitis/arthritis, while category 1 was thought to exclude the presence of manifest synovitis.
Results
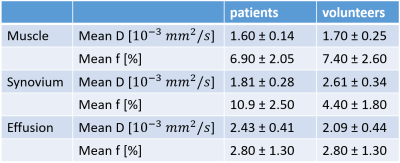
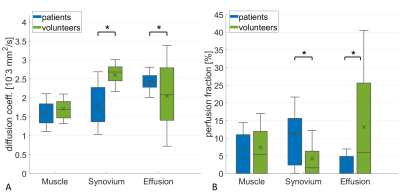
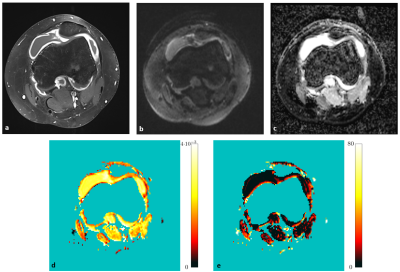
An overview of the qualitative analysis regarding presence and degree of synovitis is provided in Table 1. Figure 1 shows diffusion (A) and perfusion fraction values (B) for patients and volunteers with the quantitative data summarized in Table 2. As reference tissue, muscle shows similar values for diffusion and perfusion fraction in patients and volunteers. Significant differences were found in D and f values of synovium and effusion. In the synovium, patients show significantly (p<0.001) lower diffusion and higher perfusion fraction values, while in effusions the diffusion values were significantly lower and perfusion fraction higher than in volunteers. In the exemplary image set provided in Figure 2 a restricted diffusivity and increased perfusion fraction of the synovial layer is clearly visible in the D- and f-maps.IVIM parameters for the synovia for one of the patients classified in category 2 showed a perfusion fraction similar to those of healthy volunteers of f = 4.5%, but a diffusivity comparable to those of other patients of D = 1.6*10-3 mm2/s. Further examination revealed the cause to be periodic fever syndrome instead of JIA.
Discussion and conclusion
Mean D- and f-values agree well with previously reported work on children with JIA and at 1.5 T [3]. Significantly lower diffusion values were detected in the synovium of patients than in healthy volunteers, indicating a pathologically restricted diffusion of water molecules due to inflammatory processes. Consequently, significantly higher synovial perfusion values could be observed in patients than in volunteers due to increased mircoperfusion of the inflamed synovial layer. For the knees of the volunteers, naturally showing no or only slightly increased intraarticular fluid, the direct comparison of effusion values between the groups is somewhat critical, although there was significant difference in both D and f. For a physiological explanation, perfusion fraction f in effusion should be expected to be low to zero because there are no vessels in the joint fluid. Measurement of f in the often only slightly increased synovial fluid of healthy volunteers led to even higher values. This is most likely due to partial volume effects caused by the synovium directly adjacent to the small amount of effusion.In conclusion, DWI with IVIM imaging remains a promising alternative to contrast-enhanced imaging in pediatric patients to reliably diagnose, or rule out, synovitis of the knee joint.
Acknowledgements
The authors thank the Ulm University Center for Translational Imaging MoMAN for its support.References
[1] Le Bihan D. et. al. MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology (1986) 161 (2): 401–7.
[2] Sigmund E.et al. Intravoxel incoherent Motion (IVIM) imaging of tumor microenvironment in Locally Advanced Breat Cancer: Magn: Reson. Med. 2011 65(5):1437-1447
[3] Hilbert F. et.al. Intravoxel incoherent motion magnetic resonance imaging of the knee joint in children with juvenile idiopathic arthritis. Pediatr. Radiol. (2017) 47:681-690
Figures