0695
Use of Double-Echo Steady-State (DESS) sequence in the evaluation of pudendal nerve- A pilot trial.1Radiology, Loyola University Medical Center, Maywood, IL, United States, 2Biostatistics, Stritch School of Medicine, Maywood, IL, United States, 3Physical Medicine and Rehabilitation, Loyola University Medical Center, Maywood, IL, United States, 4Radiology and Nuclear Medicine, Loyola University Medical Center, Maywood, IL, United States
Synopsis
Pudendal neuralgia is a common cause of chronic pelvic pain, especially in females. This is caused by pudendal nerve entrapment and can be a severely disabling neuropathic pain syndrome. It is currently a clinical diagnosis and most of the time a diagnosis of exclusion without definitive imaging criteria. We retrospectively compared DESS with the routine T2, T1 and DWI described in literature for the evaluation of pudendal nerves in patients with unresolved pelvic pain. Our study showed that DESS is effective and better than T2 and DWI combined sequences for diagnosing pudendal neuropathy.
Introduction
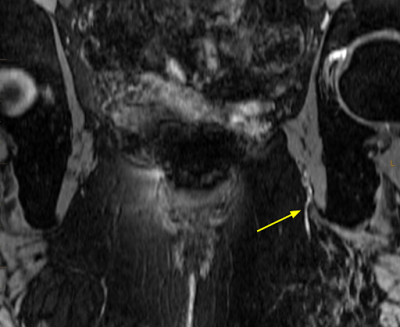
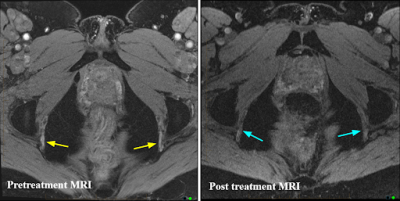
Chronic pelvic and perineal pain is a common cause of morbidity in the adult population and is usually multifactorial. One of the common causes is pudendal neuralgia caused by pudendal nerve entrapment, and usually chronic resulting in severely disabling neuropathic pain syndrome. It is reported higher in women with an incidence of 1%-4% in the general population, though this is likely much higher due to the often unrecognized and undertreated nature of the condition. Historically, pudendal neuralgia has been evaluated by clinical examination and is a diagnosis of exclusion. Treatment with nerve block injections in most cases are performed without image guidance and have variable results depending on the extent and course of nerve involvement. MRI evaluation has been performed with the routine T1, T2, and STIR sequences, describing abnormal thickening and high signal of the nerves on STIR and T2-weighted images however, there are no large studies that describe the size criteria for an abnormal nerve.3D Double-Echo Steady State (DESS) sequence, that is typically used for MSK applications for cartilage evaluation, is proven to have a high signal-to-noise ratio (SNR) due its prolonged and unbalanced readout gradient, generating two echoes before and after a spoiler gradient. The contrast in DESS is highly superior to other sequences and can aid in morphological assessment. Recently, it has been used in the evaluation of lumbosacral plexus by suppressing vessel signals, which usually confounds the signal of the nerve as they course adjacent to each other. This capability of DESS aids in a confident evaluation of nerves and can be vital especially in the evaluation of smaller peripheral nerves like the pudendal nerve, which courses alongside the pudendal vessels of similar caliber and can cause confusion in the evaluation as the nerves and vessels to elicit high signal on the aforementioned T2 and STIR sequences that have been described in the literature.
With this study, we aim to evaluate how the 3D DESS sequence, along with the routine T1, T2, and DWI can be used to evaluate the pudendal nerve.
Methods
This is an Institutional Review Board-approved, retrospective review of MR pelvis examinations of patients performed between November 2020 and October 2021. Patients >18 years with chronic pelvic pain and who had dedicated institutional MR pelvis neurography protocol were included in the study. The MRI protocol included sagittal T2, 3D axial DESS, T2 FS, T1 without FS, and DWI with a total scan time of 20 minutes (7 minutes for axial 3D DESS). Field of view for the DESS and T2 were mid pelvis through the S2 vertebra caudally to include the gluteal skin fold, with scan plane parallel to the pubococcygeal line. Analysis of MR pelvis examinations at our institution was performed by radiologists as a dedicated exam for evaluation of pudendal nerves. Several characteristics of the pudendal nerve were analyzed, including pudendal nerve course, thickness, and signal on different MRI sequences, as well as other incidental findings which may contribute to pelvic pain. Relevant clinical history including age, sex, type, laterality and duration of pain, numerical rating scale (NRS), prior history of pelvic trauma or surgery, medications, pelvic and perineal examination findings, prior pudendal nerve block injections, and any other treatment history was also collected. Statistical analysis was performed.Results
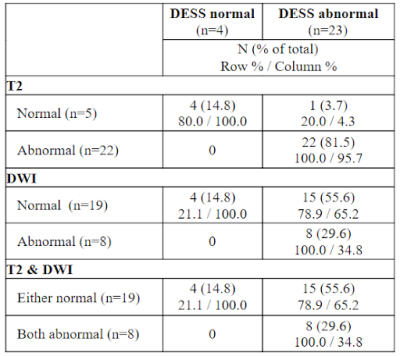
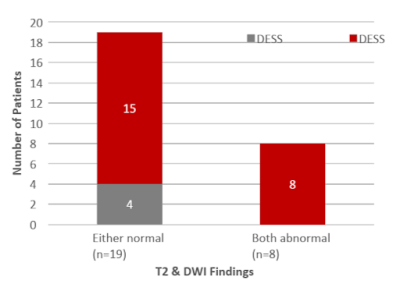
Our study included 30 patients (27 female) aged between 21-70-years-old with an average age of 50. Burning pain (46.7%) was the most common type of pain reported by patients, with pelvis (77%) and perineum (60%) being the most common sites. Sixteen patients in the cohort experienced bilateral pain (53%) and 22 patients had undergone prior pelvic or perineal surgery (73%). On MRI, 57% of patients were found to have bilateral abnormalities, 30% unilateral (20% left and 10% right), and 13% showed no abnormality. Overall, 29.6% (8/27) had both T2 & DWI abnormalities, all of whom also had DESS abnormalities detected. DESS abnormalities were more frequently detected overall (23/27, 85.2%), of which 34.8% (8/23) also had T2 & DWI abnormalities (Table 1). Additionally, thickened nerves were seen in 26 patients (87%) and distal/ terminal branches of pudendal nerve abnormality was seen in 5 patients (17%). Secondary findings of pudendal neuropathy like tortuous pudendal vessels was seen in 13% of patients.Discussion
DESS, T2, and DWI sequences were able to identify pudendal nerve abnormalities in symptomatic patients, and also quantitatively measure the pudendal nerve thickness. DESS was more effective at identifying these abnormalities than a combination of T2 + DWI imaging with a more accurate degree of pain localization than T2+DWI and also correlated better with the patient’ clinical symptoms and examination findings. Limitations of the study include small sample size and can be rectified with larger sample size in future. Plan for the future includes signal intensity measurements of the nerve relative to the adjacent vessel for quantitative diagnostic information in patients with visually mild increased signal in the abnormal nerve.Conclusion
DESS is useful in the evaluation of patients with pelvic pain, especially those with clinical signs of pudendal neuralgia. It can increase the sensitivity of imaging diagnosis and improve confidence among radiologists when added to the routine MRI protocol for peripheral nerve evaluation.Acknowledgements
NoneReferences
1. Wadhwa V, Hamid AS, Kumar Y, Scott KM, Chhabra A. Pudendal nerve and branch neuropathy: magnetic resonance neurography evaluation. Acta Radiol. 2017 Jun;58(6):726-733.
2. Soldatos T, Andreisek G, Thawait GK, Guggenberger R, Williams EH, Carrino JA, Chhabra A. High-resolution 3-T MR neurography of the lumbosacral plexus. Radiographics. 2013 Jul-Aug;33(4):967-87.
3. Chhabra A, McKenna CA, Wadhwa V, Thawait GK, Carrino JA, Lees GP, Dellon AL. 3T magnetic resonance neurography of pudendal nerve with cadaveric dissection correlation. World J Radiol. 2016 Jul 28;8(7):700-6.
4. Hough DM, Wittenberg KH, Pawlina W, Maus TP, King BF, Vrtiska TJ, Farrell MA, Antolak SJ Jr. Chronic perineal pain caused by pudendal nerve entrapment: anatomy and CT-guided perineural injection technique. AJR Am J Roentgenol. 2003 Aug;181(2):561-7.
5. Vancaillie T, Eggermont J, Armstrong G, Jarvis S, Liu J, Beg N. Response to pudendal nerve block in women with pudendal neuralgia. Pain Med. 2012 Apr;13(4):596-603.
Figures