0679
Advanced Vessel- and Cell-Size MRI to Assess Chemo-Radiation Treatment Response in Pediatric Ependymoma Models
Natalie J Serkova1, Jane S Manalo2, Jenna L Steiner2, Andrea M Griesinger2, Angela Pierce2, Mark S Brown2, and Nicholas F Foreman3
1Radiology, University of Colorado Anschutz Medical Campus, Aurora, CO, United States, 2University of Colorado Anschutz Medical Campus, Aurora, CO, United States, 3Children's Hospital Colorado, Aurora, CO, United States
1Radiology, University of Colorado Anschutz Medical Campus, Aurora, CO, United States, 2University of Colorado Anschutz Medical Campus, Aurora, CO, United States, 3Children's Hospital Colorado, Aurora, CO, United States
Synopsis
We report on an advanced mpMRI protocol for characterizing the cellular and vascular phenotype in an orthotopic mouse model of pediatric ependymoma (EPN). Using diffusion-weighted based cell-size imaging, iron-oxide based vessel-size imaging and quantitative T2-maps, we report on an EPN-specific phenotype, characterized by an increased cell size (S=14 microns), increased vessel density index (Q=0.54), and low ADC values (0.63x10-3). Radiation treatment (10 Gy) in combination with 5-fluorouracil chemotherapy resulted in a decrease of gross tumor volumes, tumor necrosis with decreased cell sizes and increased ADC values, as well as a dramatic vascular-inflammatory response (highly decreased Q and DT2 values).
Introduction
Ependymoma (EPN) is an aggressive pediatric brain tumor that contributes significantly to poor overall outcomes in children1. The benefits of chemotherapy in pediatric patients with ependymoma have not been defined2, and EPN treated with surgery and radiation therapy can still recur in 23-66% of patients3. Our group has previously established aggressive behaviors of EPN, including high tumor cellularity, cytological anaplasia, high mitotic index, tumor necrosis, and the presence of inflammatory cells such as M2-type myeloid cells4. The purpose of this study is to develop and optimize an advanced mpMRI protocol (cell-size, vessel-size and inflammation imaging) to characterize the phenotype and chemo-radiation treatment (CRT) response in an orthotopic mouse of patient-derived xenografts (PDX) of pediatric EPNMethods
All animal protocols were reviewed and approved by the University of Colorado IACUC. Female severely immune deficient (SCID) mice were used for intracranial orthotopical inoculation of disaggregated tumors from pediatric EPN patients (n=22). Once the intracranial tumor reached at least 5 mm3, the animals were assigned to a placebo and CRT groups (10 Gy radiation plus 30 mg/kg 5-fluorouracil, Figure 1). All radiation treatment was perform of the animal image-guided precision XRAD irradiator, using MRI and CT guided EPN localization. For each MRI session, the animal were inserted into a Bruker 9.4 Tesla BioSpec MRI scanner with a Bruker mouse head array RF cryo-coil. Each session consisted of an mpMRI protocol based on the following optimized sequences: - high resolution T2w turboRARE (sagittal and axial) for tumor volume; - diffusion weighted imaging (DWI) for tumor necrosis and edema; - selective size imaging using filters via diffusion times (SSIFT); - vessel size imaging (VSI) (fast T2* during 10 mg/kg iron-oxide ferumoxytol injection); - quantitative T2maps (qT2) for inflammation (before and 24hr after ferumoxytol injection). Total acquisition time was 32 minutes based on high-resolution T2w turboRARE (3D, 5min30s), fast spin echo diffusion weighted imaging with 6 b-values (DWI axial, 1min30s), quantitative MSME T2 maps with 8 echoes before and after ferumoxytol (iron oxide SPION) administration (qT2maps axial, 10min), and R2 and R2* maps (each 7min30sec). Analytical methodologies included (i) conventional volumetric analysis, apparent diffusion coefficient (ADC) values and T2 relaxation times using ParaVision NEO software; in-house MATLAB simulations to calculate SSIFT iAUC, vessel size imaging (VSI) and density indices (Q) VSI = 0.424(D/gDcB0)1/2 (DR2*/DR2)3/2 [mm] and Q = DR2/(DR2*)2/3 [sec-1/3] The qT2 were repeated 24 hours after SPION injection. This protocol was performed before CRT, immediately after CRT, and two weeks after CRT.Results
High-resolution turboRARE T2w-MRI (48 microns in-plane resolution) clearly showed that all EPN PDX were inoculated and homed at the proper anatomical location for EPN, the cerebellum (Figure 2). The sensitivity of T2w-MRI scans was 0.2 mm for the smallest tumor detected; the median tumor volumes at the baseline were 21±12 mm3. They also revealed increased blood vessel densities (0.54±0.12), high SSIFT iAUC (7.1±1.2) indicative for EPN cell size of 14±3 microns, and low ADC values (as low as 0.58x10-3 mm2/s) in EPN as compared to the normal cerebellum. The 5-day CRT with 2Gy/day and 30 mg/kg 5-FU resulted in a significant decrease in the tumor volumes (Figure 2), accompanied by the increased ADC values and decreased SSIFT iAUC and cell size two weeks after CRT (Figure 3). Interestingly, the most immediate response, seen on ferumoxytol-enhanced VCI and qT2 (-4 ms median), seen as soon as 2 days after the CRT, was related to a decreased blood vessel density and an increased presence of inflammatory macrophages and microglial cells in irradiated EPN (Figure 4).Discussion
Orthotopically implanted PDX EPN xenografts closely mimic histological features, anatomical location and radiological features of the primary tumors. Our advanced mpMRI protocol followed by novel MATLAB algorithm analysis allows for a unique characterization of pediatric EPN as well as assessing the tumor response to a clinically relevant CRT protocol in a mouse model. A significant decrease in vessel size density and an increase in inflammatory cells were seen as soon as 2 days after CRT. The late response (2 weeks post CRT) is characteristic by decreased ADC values and cell size, resulting in significantly decreased tumor volumes.Summary
We successfully developed a comprehensive mpMRI protocol for an orthotopic pediatric EPN model, which can be readily translated into human imaging. In addition to the volumetric MRI assessment, we introduce cell size imaging based on the intrinsic distinguishing feature between cancerous (14 microns) and normal brain cell (5 microns). The relation of ferumoxytol-enhanced transverse relaxation rates R2* and R2 provides in vivo VSI mapping of the mean caliber of cerebral vessels, while decreased T2 values in qT2 are reflective for iron accumulation in inflammatory cells such as macrophages and microglial cells immediately after CRT.Acknowledgements
The study was supported by the NIH Shared Instrumentation Grant Program (S10 OD023485 and S10 OD027023), the University of Colorado Cancer Center grant (P30 CA046934), and Michele Plachy-Rubin Pilot Grant ProgramReferences
1. Merchant TE. Current Clinical Challenges in Childhood Ependymoma: A Focused Review. J Clin Oncol. 2017;35: 2364-2369. 2. Timmermann B, Kortmann RD, Kuhl J, et al. Role of radiotherapy in anaplastic ependymoma in children under age of 3 years: results of the prospective German brain tumor trials HIT-SKK 87 and 92. Radiother Oncol. 2005;77: 278-285. 3. Byer L, Kline CN, Coleman C, Allen IE, Whitaker E, Mueller S. A systematic review and meta-analysis of outcomes in pediatric, recurrent ependymoma. J Neurooncol. 2019;144: 445-452. 4. Pierce AM, Witt DA, Donson AM, et al. Establishment of patient-derived orthotopic xenograft model of 1q+ posterior fossa group A ependymoma. Neuro Oncol. 2019;21: 1540-1551.Figures
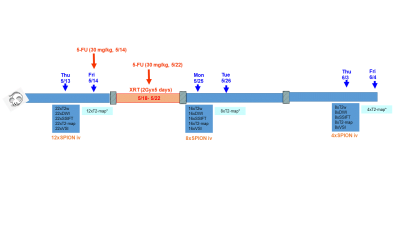
Figure 1: Timeline for Cell Size Imaging (CSI), Vessel Size Imaging (VSI) and
Inflammation MRI for orthotopic pediatric ependymoma tumors
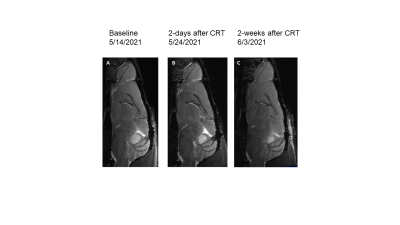
Figure 2: T2w sagittal turboRARE shows reduced
tumor volume over time, indicating efficacy of RT+5FU treatment
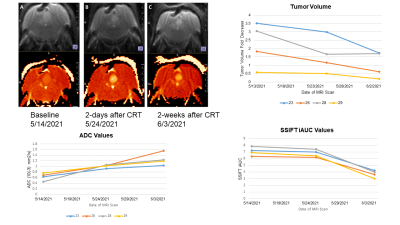
Figure 3: Changes in DWI, ADC, and SSIFT iAUC two
weeks after chemo-radiation (RT+5FU) treatment in a mouse EPN PFX model
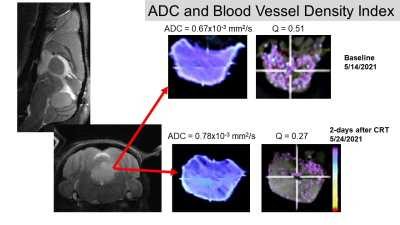
Figure
4: Changes in VSI (vessel density index Q) only two days after chemo-radiation
(RT+5FU) treatment in a mouse EPN PFX model
DOI: https://doi.org/10.58530/2022/0679