0659
Hyperpolarized 129Xe MR Imaging in Neonates with Bronchopulmonary Dysplasia: Feasibility and Challenges1POLARIS, Imaging Sciences, Department of Infection, Immunity & Cardiovascular Disease, The University of Sheffield, Sheffield, United Kingdom, 2Center for Pulmonary Imaging Research, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 3Division of Pulmonary Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 4Department of Radiology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 5Department of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, OH, United States, 6The Perinatal Institute, Section of Neonatology, Perinatal and Pulmonary Biology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 7Division of Respiratory Care, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States, 8GE Healthcare, Munich, Germany
Synopsis
We report the first-ever experience in performing HP 129Xe MRI in neonates. The neonates had prematurity-related lung disease (bronchopulmonary dysplasia), a major cause of morbidity/mortality that remains poorly characterised. The feasibility of imaging during a short (<3s) breath-hold apnea was demonstrated. Spiral-based 129Xe ventilation imaging showed good image quality (SNR>20) and sufficient sensitivity to detect mild ventilation abnormalities. Dynamic 129Xe spectroscopy revealed the existence of resonances near the conventional tissue/plasma and red blood cells resonances observed in children and adults. With further data, our work may impact on the management of infant lung diseases in the neonatal period and beyond.
Introduction
Bronchopulmonary dysplasia (BPD) is a chronic lung disease and major cause of morbidity/mortality in pre-term infants but remains poorly characterised. Free-breathing, retrospectively-gated 3D radial 1H ultra-short echo time (UTE) MRI has been demonstrated as a safe, non-ionizing alternative to CT for visualizing structural lung disease in neonates with BPD, with UTE-derived biomarkers correlating to clinical outcomes1. However, UTE provides limited information on lung function, and conventional pulmonary function testing poses technical and safety challenges in infants.Hyperpolarized (HP) 129Xe MRI is a safe, sensitive means to assess lung function, including ventilation, microstructure and gas exchange, in adult and pediatric populations2. One proof-of-concept study reported preliminary 3He gas findings3, but HP 129Xe gas MRI in infants has not been explored, and maintaining a coordinated breath-hold apnea is challenging. Recent work has shown that HP 129Xe MRI can detect long-term functional lung changes in children born pre-term assessed at school age4. It is therefore vital to be able to detect such changes in early life to guide patient management. Here, we report our initial experience in performing HP 129Xe MRI in neonates with BPD.
Methods
Prior to MRI, the feasibility of a 3-second induced breath-hold apnea in nine infants with and without lung disease aged 0—5 months was assessed using inhaled nitrogen gas at bedside. There were no adverse events or significant changes in heart rate; in some infants a ~5% drop in SpO2 ~20s post-breath-hold was observed, which recovered within a few seconds.Separately, two preterm male neonates with severe BPD on nasal cannula (born a) 26 and b) 24 weeks post-menstrual age, imaged at 38 and 41 weeks, respectively) were recruited for MRI, with parental consent and IRB approval from Cincinnati Children’s. MRI was performed on a multi-nuclear 1.5T neonatal-sized MRI system5 using a 129Xe/1H switched frequency high-pass birdcage coil6 (Figure 1). 129Xe ventilation images were acquired using 2D slice-selective spoiled gradient echo sequences, with either a sequential Cartesian readout (FOV:24cm, resolution:3.75x3.75x9.0mm, FA:11°, ~0.5s per slice) or spiral readout (FOV:24cm, resolution:3x3x7.5mm, 12 arms, FA:20°, ~0.2s per slice). In subject b) dynamic dissolved-phase 129Xe spectroscopy was performed7 (BW:31.25kHz, resolution:61Hz/pt, FA:20° frequency-selective RF pulse, TR:25.7ms).
For all acquisitions, pure 129Xe polarized to ~40% was delivered using a facemask via Tedlar bag compression at 15cm H2O by a neonatologist. Breath-hold apnea of ≤3 s was induced. Data were acquired repeatedly during and after the breath-hold (total period of ≥10s). To provide complementary high-quality structural images, 3D radial 1H UTE data were acquired during tidal breathing8 (resolution:0.7mm3).
Results
Heart-rate and SpO2 were within 40 bpm and 8% of baseline 2 minutes post-inhalation, with no safety concerns at follow-up. Image quality obtained from conventional Cartesian SPGR acquisitions was poor, with inconsistent signal appearance across slices (Figure 2). Spiral acquisitions showed good image quality across several temporal phases (Figure 3); SNR of the averaged image derived from the first 5 dynamics was 24.8±2.4. Qualitatively, a region of trapped gas on UTE MRI appears to spatially correspond to a ventilation defect on 129Xe MRI (red arrows), and additional ventilation abnormalities with no apparent accompanying structural abnormality were observed (e.g. green arrow). Dynamic 129Xe spectroscopy revealed the existence of resonances near the conventional tissue/plasma (TP) and red blood cells (RBC) resonances observed in pediatric and adult populations, which persisted throughout the breath-hold duration. The mean spectrum in this N=1 study indicates a low apparent RBC resonance at ~221ppm and possible sub-structure to the apparent TP peak at ~194 ppm. The mean RBC/TP signal ratio was ~0.24 (c.f. ~0.5 for healthy adults)).Discussion
Whilst interpretation of the clinical significance of our findings is limited by small N, it is encouraging that HP 129Xe MRI shows sensitivity to minor ventilation abnormalities in this population. The observation of a low RBC component relative to TP and Gas, and possible sub-structure / temporal variations in the TP peak in dissolved-phase 129Xe spectroscopy are inconclusive, but the SNR is sufficient that the spectral appearance of fetal hemoglobin and its differences to adult hemoglobin could eventually be investigated.Challenges: sequential Cartesian SPGR sequences appear unsuitable for imaging this population, where motion and incomplete apnea will be common; there is a need for high SNR and k-space encoding efficiency sequences (e.g. spiral), wherein the center of k-space is sampled regularly. Gas delivery is a major determinant of image quality, and whilst we have demonstrated that a short breath-hold apnea procedure is feasible in infants, maintaining the desired pressure through the facemask was challenging and often the images indicated gas not reaching the lung region. A tailored free-breathing approach with HP 129Xe and O2 mixtures may offer a more robust gas-delivery solution.
Conclusion
We have demonstrated that inhaled 129Xe MRI is feasible in neonates using a short breath-hold apnea technique. It is early to draw clinically-relevant conclusions, but initial observations of minor ventilation abnormalities apparently unassociated with structural pathology, and potential differences in the dissolved-phase 129Xe resonance structures compared with older children and adults, are promising. With further data in neonates with a range of BPD severities, we anticipate potential implications on the management of infant lung diseases and avenues for longitudinal monitoring in the neonatal period and beyond.Acknowledgements
We acknowledge funding from NIH R01 HL146689, Cincinnati Children’s Research Foundation, European Respiratory Society (ERS) fellowship (RESPIRE3), European Commission Horizon 2020 grant agreement ID: 713406, Thrasher Research Fund Early Career Award. We also thank Prof Bastiaan Driehuys for the provision of a multi-nuclear RF amplifier.
References
[1] N. S. Higano, D. R. Spielberg, R. J. Fleck, et al. Am J Respir Crit Care Med. 2018, 198, 1302-11.
[2] N. J. Stewart, L. J. Smith, H. F. Chan, et al. Br J Radiol. 2021, 94, 20210207.
[3] T. A. Altes, C. H. Meyer, J. F. Mata, et al. Clinical Imaging. 2017, 45, 105-10.
[4] J. M. Wild, A. Biancardi, H.-F. Chan, et al. European Respiratory Journal. 2019, 54, PA3171.
[5] J. A. Tkach, S. L. Merhar, B. M. Kline-Fath, et al. American Journal of Roentgenology. 2013, 202, W95-W105.
[6] R. Pratt, R. Giaquinto, W. Loew, et al. Proceedings of the International Society for Magnetic Resonance in Medicine (ISMRM) Annual Meeting. 2021, 3563.
[7] E. A. Bier, S. H. Robertson, G. M. Schrank, et al. NMR Biomed. 2019, 32, e4029.
[8] N. S. Higano, A. D. Hahn, J. A. Tkach, et al. Magn Reson Med. 2017, 77, 1284-95.
Figures
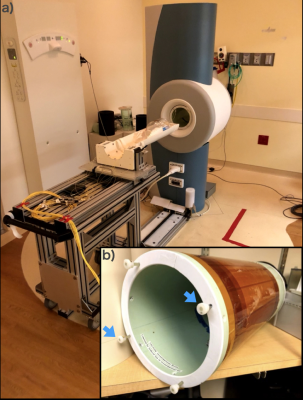
Figure 1: a) MRI system used for multi-nuclear MRI in neonates; small bore 1.5T, situated within the neonatal intensive care unit, b) Switchable 129Xe/1H high-pass birdcage coil; insertion or removal of rods (blue arrows) adds or subtracts capacitance, respectively, to the resonance circuit to alter the resonant frequency without repositioning the neonatal patient.
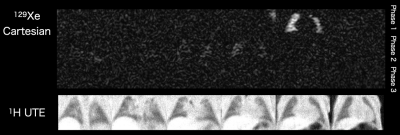
Figure 2: Time-series of 129Xe Cartesian SPGR ventilation images (6 slices) in subject a) during and shortly after a ~3s breath-hold apnea period (time to acquire all slices for each phase; 𝛥t~3 s), demonstrating inconsistent signal detection across slices. Approximately corresponding slices from free-breathing 1H UTE MRI are shown below.
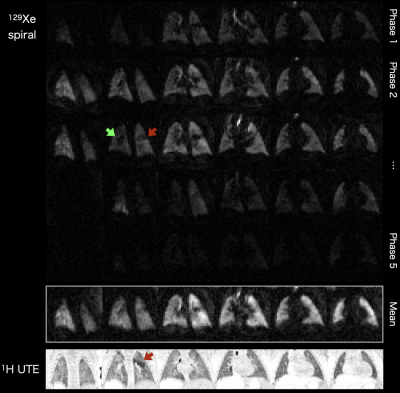
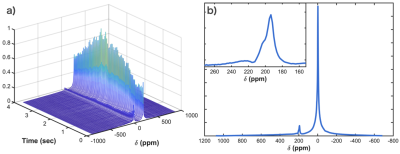
Figure 4: a) MR spectroscopy time series of 129Xe in the lungs of subject b), showing the time-course of the gas- and dissolved-phase resonances during and shortly after a 3-second breath-hold apnea period; centered on the dissolved-phase. b) Average of the spectra shown in a) after discarding the first 50 FIDs (0 ppm: calibrated 129Xe gas resonance). Inset: magnified view of the dissolved-phase resonances, indicating an apparent peak at ~194 ppm (possible “side” peak at ~202 ppm, which may indicate a frequency drift during the acquisition), and an apparent peak at ~221 ppm.