0612
Hyperperfusion on arterial spin labelling is associated with cognitive impairment in infants with neonatal hypoxic ischemic encephalopathy1Center for MR Research, University Children's Hospital, Zurich, Switzerland, 2Radiology, University Children's Hospital, Zurich, Switzerland, 3Neonatology and Pediatric Intensive Care, University Children's Hospital, Zurich, Switzerland, 4Anaesthesia, University Children's Hospital, Zurich, Switzerland, 5Child Development Center, University Children's Hospital, Zurich, Switzerland
Synopsis
Neonatal hypoxic ischemic encephalopathy (HIE) is a serious neurological condition, representing a primary cause of neonatal death and developmental impairment. In newborns with HIE, hyperperfusion is related to severe adverse outcomes, but less is known about the link between perfusion and mild to moderate developmental impairments. Using a voxelwise correlation analysis, we investigated the link between ASL perfusion in newborns with HIE and developmental outcome at 2 years. A more adverse outcome was associated with hyperperfusion across the whole brain. A better cognitive outcome was associated with lower perfusion in the bilateral basal ganglia, thalamus, hippocampus and cerebellum.
Introduction
Neonatal hypoxic ischemic encephalopathy (HIE) is a serious neurological condition, representing one of the primary causes of neonatal death and developmental impairment. Cerebral hyperperfusion has been demonstrated following HIE both in animals and in humans1. In newborns with HIE, hyperperfusion has been related to severe adverse outcomes such as death or severe disability2, but less is known about the link between perfusion and mild to moderate developmental impairments. While newborns with severe HIE are at highest risk of severe disability3, newborns with mild or moderate HIE demonstrate a wide spectrum of cognitive and behavioural outcomes4. The purpose of the present study was to investigate the link between cerebral perfusion in newborns with neonatal HIE, assessed with arterial spin labelling (ASL), and neurodevelopmental outcome at two years. Based on previous reports2 we hypothesised that increased perfusion would be associated with lower motor, cognitive, and language outcome scores from a standardised neurodevelopmental assessment, as well as with impairments in multiple neurodevelopmental domains.Methods
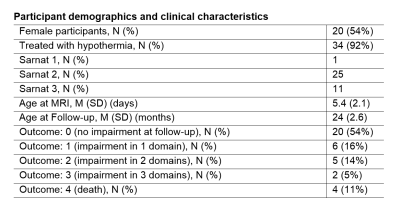
The participant group consisted of 37 term-born neonates (see table 1 for demographics), referred for MRI as part of a clinical evaluation for HIE. 34/37 neonates were cooled with hypothermia. Arterial spin labelled (ASL) perfusion MRI data were collected with a 3D background-suppressed, pseudocontinuous ASL sequence. 28 infants were scanned with a 3T GE MR750 scanner (GE Healthcare, Milwaukee, WI, USA), while the remaining infants were scanned with 3T GE HD.xt (n=8) or 1.5T GE MR450 (n=1) scanners. A post-labelling delay of 2 seconds was used at 3T and 1.5 seconds was used at 1.5T. Perfusion was quantified using the default model implemented in the online perfusion reconstruction provided by the scanner vendor, accounting for differences in blood T1 between 1.5T and 3T. Perfusion maps were normalised to a neonatal perfusion template using FSL-FLIRT, and voxelwise perfusion was compared to the neurodevelopmental outcome using FSL-randomise, covarying for the scanner on which the ASL data were acquired, and controlling for multiple comparisons with threshold free cluster enhancement (TFCE).A neurodevelopmental assessment was performed at 2 years as part of a structured follow-up program by a developmental paediatrician or paediatric neurologist, using the Bayley scales of infant and toddler development, 3rd version (n=35), the Bayley-II (n=1), or the Griffiths neurodevelopmental assessment (n=1). Outcome was categorised as: 0 (no impairment observed), 1 (impairment in one domain), 2 (impairment in two domains), 3 (impairment in 3 domains) or 4 (death). For each domain, impairment was defined by a composite score of less than 85 for the Bayley-III or less than 70 for the Bayley-II.5 Permutation testing was performed to test for statistically significant voxelwise correlations between the perfusion and outcome index, and the composite scores for the individual Bayley-III cognitive, language, and motor domains. (For the patient assessed with the Bayley-II, the cognitive score was converted to a Bayley-III cognitive composite score6). The significance threshold was set to p<0.05, TFCE corrected.
Results
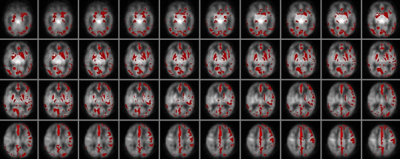
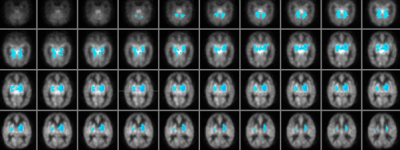
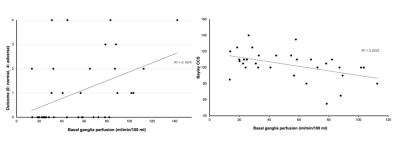
20 of the 37 infants (54%) demonstrated a normal outcome, while six showed a mild impairment in language development (Bayley-III language composite scores of 78-84), but normal cognitive and motor development. Five infants showed impairment in two domains, two showed impairment in all three domains, and four infants died.In the voxelwise correlation analysis, a more adverse outcome was associated with increased perfusion bilaterally in the basal ganglia and a diffuse set of regions distributed across all cortical lobes, suggestive of a global rather than regional association between perfusion and outcome (Figure 1). Voxelwise correlation analyses between perfusion and the individual Bayley-III composite scores revealed a significant association between cognitive outcome and perfusion in the bilateral basal ganglia, with clusters extending into the thalamus, hippocampus and the anterior part of the superior cerebellum (Figure 2). Scatter plots depicting the association between perfusion and outcome or cognitive score are shown in Figure 3. No significant correlations were observed between perfusion and motor or language outcome, after correction for multiple comparisons.
Discussion
The link between basal ganglia hyperperfusion and severe adverse outcome from HIE has been described previously,2 but the present study extends these findings by demonstrating firstly that the correlation between perfusion and adverse outcome appears to represent a global effect, and secondly, that elevated perfusion is also linked to mild or moderate impairment as well as severe adverse outcomes. The latter observation is of high clinical relevance, given the broad spectrum of outcomes observed in infants with moderate HIE, and the need for imaging biomarkers for outcome in in this population. Unlike results from another recent HIE perfusion study7, we did not observe a link between perfusion and motor or language outcome, but the correlation analyses revealed an association between cognitive outcome and regional perfusion in the basal ganglia, hippocampus, and cerebellum. To our knowledge, this association has not been described previously, and underscores the importance of subcortical and cerebellar regions for cognitive as well as motor development during the neonatal period.Conclusion
In a cohort of HIE infants with predominantly moderate HIE, global hyperperfusion was associated with an adverse outcome, and a better cognitive outcome was linked to lower perfusion in the basal ganglia, thalamus, hippocampus, and cerebellum..Acknowledgements
The authors would like to acknowledge Annette Hackenberg for assistance with some of the outcome assessments. This work was funded by a grant from the UBS foundation, Zurich, SwitzerlandReferences
1Kleuskens DG, Gonçalves Costa F, Annink KV, van den Hoogen A, Alderliesten T, Groenendaal F, Benders MJN and Dudink J (2021) Pathophysiology of Cerebral Hyperperfusion in Term Neonates With Hypoxic-Ischemic Encephalopathy: A Systematic Review for Future Research. Front. Pediatr. 9:631258. doi: 10.3389/fped.2021.631258
2De Vis JB, Hendrikse J, Petersen ET, de Vries LS, van Bel F, Alderliesten T, Negro S, Groenendaal F, Benders MJ. Arterial spin-labelling perfusion MRI and outcome in neonates with hypoxic-ischemic encephalopathy. Eur Radiol. 2015 Jan;25(1):113-21. doi: 10.1007/s00330-014-3352-1
3Pierrat V, Haouari N, Liska A, Thomas D, Subtil D, Truffert P; Groupe d'Etudes en Epidémiologie Périnatale. Prevalence, causes, and outcome at 2 years of age of newborn encephalopathy: population based study. Arch Dis Child Fetal Neonatal Ed. 2005 May;90(3):F257-61
4van Handel M, Swaab H, de Vries LS, Jongmans MJ. Long-term cognitive and behavioral consequences of neonatal encephalopathy following perinatal asphyxia: a review. Eur J Pediatr. 2007;166(7):645-654. doi:10.1007/s00431-007-0437-8
5Bach AM, Fang AY, Bonifacio S, Rogers EE, Scheffler A, Partridge JC, Xu D, Barkovich AJ, Ferriero DM, Glass HC, Gano D. Early Magnetic Resonance Imaging Predicts 30-Month Outcomes after Therapeutic Hypothermia for Neonatal Encephalopathy. J Pediatr. 2021 Nov;238:94-101.e1
6Jary S, Whitelaw A, Walloe L, Thoresen M. Comparison of Bayley-2 and Bayley-3 scores at 18 months in term infants following neonatal encephalopathy and therapeutic hypothermia. Dev Med Child Neurol. 2013 Nov; 55(11): 1053–1059.
7Zheng Q, Martin-Saavedra JS, Saade-Lemus S, Vossough A, Zuccoli G, Gonçalves FG, Freeman CW, Ouyang M, Singh V, Padula MA, Demauro SB, Flibotte J, Eichenwald EC, Detre JA, Sze RW, Huang H, Hwang M. Cerebral Pulsed Arterial Spin Labeling Perfusion Weighted Imaging Predicts Language and Motor Outcomes in Neonatal Hypoxic-Ischemic Encephalopathy. Front Pediatr. 2020 Sep 25;8:576489
Figures