0609
Deep Learning Reconstruction: Clinical Utility for 3D MRCPs Obtained by Different k-Space Data Acquisition Methods in IPMN Patients1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Radiology, Fujita Health University Hospital, Toyoake, Japan
Synopsis
We hypothesized that deep learning reconstruction (DLR) and multiple k-space data by means of each of the repetition time (TR) techniques (Fast 3D mode multiple: Fast 3Dm) are more useful than parallel imaging (PI) and compressed sensing (CS) for shortening acquisition time and improving image quality and IPMN evaluation capability on 3D MRCP. The purpose of this study was thus to compare the utility of DLR used for PI, Fast 3Dm and CS for improvement of acquisition time, image quality and IPMN evaluation capability on 3D MRCP for patients with IPMN.
Introduction
Pancreatic intraductal papillary mucinous neoplasms (IPMNs) possess malignant potential and feature a broad histological spectrum, ranging from low-grade to high-grade dysplasia, and even to invasive carcinoma1, 2. Regular surveillance is therefore important to determine the appropriate surgical indications, and magnetic resonance imaging (MRI) is the preferred imaging modality rather than computed tomography (CT)3. Moreover, three-dimensional (3D) magnetic resonance cholangiopancreatography (MRCP) is considered one of the key techniques in this setting. Parallel imaging (PI) and compressed sensing (CS) have been suggested as useful for improving temporal or spatial resolutions since 2004. Recently, Canon Medical Systems Corporation has clinically introduced a new k-space data acquisition method as Fast 3D mode, which is acquired multiple k-space data by means of each of the repetition time (TR) techniques (Fast 3D mode multiple: Fast 3Dm). Moreover, deep learning reconstruction (DLR) method has been suggested as useful for image quality improvement at different imaging areas4, 5. However, no reports have been published for demonstrating the utility of DLR for image quality and diagnostic performance improvements on 3D MRCP obtained by different k-space methods in patients with IPMNs. We hypothesized that DLR and Fast 3Dm are more useful than PI and CS with PI for shortening acquisition time and improving image quality and IPMN evaluation capability on 3D MRCP. The purpose of this study was thus to compare the utility of DLR used for PI, Fast 3Dm and CS for improvement of acquisition time, image quality and IPMN evaluation capability on 3D MRCP for patients with IPMN.Materials and Methods
Thirty-two IPMN patients who had undergone 3D MRCPs obtained with PI (SPEEDER, Canon Medical Systems), Fast 3Dm and CS (Compressed SPEEDER, Canon Medical Systems) at two 3T system (Vantage Centurian, Canon Medical Systems) and reconstructed with and without DLR (Advanced intelligent Clear-IQ Engine: AiCE) were retrospectively included in this study. Acquisition time of each MRCP protocol was also recorded. Results of endoscopic ultrasound, endoscopic retrograde cholangiopancreatography (ERCP), surgery or pathological examination were determined as standard reference. For quantitative image quality evaluation, signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) of common bile duct (CBD) and main pancreatic duct (MPD) obtained with all protocols were evaluated. For qualitatively assessments for image quality and IPMN subtype classification, each evaluation was performed by two investigators with 7 and 27-year experiences, and each final evaluation was determined by consensus of two readers. Mean examination times of the 3D MRCP protocol were compared among all sequences with and without DLR by means of Tukey’s honestly significant difference (HSD) test. To compare quantitative image quality indexes among all 3D MRCP sequences with and without DLR, SNR and CNR were compare among all methods by means of Tukey’s HSD test. Inter-observer agreement for overall image quality and IPMN subtypen classification of each 3D MRCP protocol were evaluated by using weighted kappa statistics and χ2 test. Then, IPMN subtype classification accuracy with standard reference was compared among all methods by means of McNemar’s test.Results
Representative case is shown in Figure 1. In 32 IPMN patients, 50 IPMNs (main ductal type: n=12, secondary pipeline type: n=30, mixed type: n=8) were diagnosed. A comparison of mean examination times of all 3D MRCP protocols showed that mean examination times of Fast 3Dm and CS reconstructed with and without DLR were significantly shorter than those of PI with and without DLR (p<0.05). Comparison of results for SNR and CNR on all methods are shown in Figure 2. SNR and CNR of each sequence with DLR were significantly higher than of those without DLR (p<0.05). Moreover, SNR and CNR of 3D MRCP for PI with DLR and Fast 3D with DLR were significantly higher than those for CS without DLR (p<0.05). Inter-observer agreement for overall image quality of each 3D MRCP protocol was assessed as significant and substantial (0.64£κ£0.79, p<0.0001). Inter-observer agreements for IPMN subtype classification were assessed as significant and almost perfect (0.93£κ£0.98, p<0.0001). Comparisons of overall image quality and IPMN subtype classification generated by all methods are shown in Figure 3. Overall image quality obtained with each 3D MRCP protocol with DLR were significantly higher than of those without DLR (p<0.05). Overall image quality of 3D MRCPs using PI and Fast 3Dm with DLR were significantly higher than those of others (p<0.05). However, there were no significant difference of IPMN subtype classification among all MRCPs (p>0.05).Conclusion
DLR is useful for improving image quality on 3D MRCP obtained with PI, Fast 3Dm or CS, although there were no significant difference for IPMN evaluation. Moreover, Fast 3Dm is considered as more useful than PI and CS for MRCP in patients with IPMN.Acknowledgements
This study was technically and financially supported by Canon Medical Systems Corporation.References
- Basturk O, Hong SM, Wood LD, et al. A Revised Classification System and Recommendations From the Baltimore Consensus Meeting for Neoplastic Precursor Lesions in the Pancreas. Am J Surg Pathol. 2015;39(12):1730-1741.
- Tanaka M, Fernández-Del Castillo C, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017;17(5):738-753.
- European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018;67(5):789-804.
- Kidoh M, Shinoda K, Kitajima M, et al. Deep Learning Based Noise Reduction for Brain MR Imaging: Tests on Phantoms and Healthy Volunteers. Magn Reson Med Sci. 2020; 19(3): 195-206.
- Ueda T, Ohno Y, Yamamoto K, et al. Compressed sensing and deep learning reconstruction for women's pelvic MRI denoising: Utility for improving image quality and examination time in routine clinical practice. Eur J Radiol. 2021;134:109430.
Figures
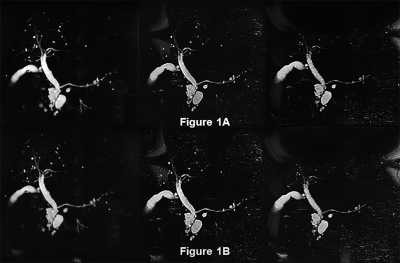
Figure 1. An 81-year-old female patient with IPMN (L to R: 3D MRCPs using PI, Fast 3Dm and CS reconstructed with DLR [Fig. 1A] and without DLR [Fig. 1B])
IPMNs also demonstrated as secondary pipeline-type multifocal sites on all sequences. The pancreaticobiliary tree and MPD visualizations on 3D MRCP using CS reconstructed with and without DLR were slightly inferior to those of other k-space acquisition methods with and without DLR. In addition, DLR was improved visualization level on MRCP obtained by each method.
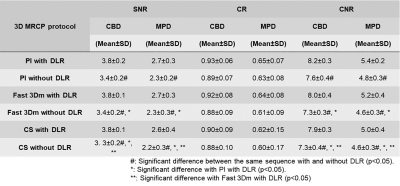
Figure 2. Comparison of results for SNR and CNR on all MRCPs.
SNRs and CNRs of each sequence with DLR were significantly higher than of those without DLR (p<0.05). Moreover, SNRs and CNRs of 3D MRCP for PI with DLR and Fast 3D with DLR were significantly higher than those for CS without DLR (p<0.05).
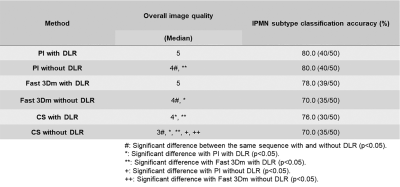
Figure 3. Compared results of overall image quality and IPMN subtype classification accuracy among all MRCPs.
Overall image quality obtained with each 3D MRCP protocol with DLR were significantly higher than of those without DLR (p<0.05), although there was no significant difference of IPMN subtype classification among all MRCPs (p>0.05). Moreover, overall image quality of 3D MRCPs using PI and Fast 3Dm with DLR were significantly higher than those of others (p<0.05).