0381
High resolution CINE imaging of guided knee motion using golden-angle radial MRI and a novel knee loading device
Martin A Aleksiev1, Martin Krämer2, Nicholas M Brisson3, Marta B Maggioni1, Georg N Duda3, and Jürgen R Reichenbach1
1Medical Physics Group, Institute of Diagnostic and Interventional Radiology, Jena University Hospital - Friedrich Schiller University Jena, Jena, Germany, 2Institute of Diagnostic and Interventional Radiology, Jena University Hospital - Friedrich Schiller University Jena, Jena, Germany, 3Julius Wolff Institute, Berlin Institute of Health at Charité - Universitätsmedizin Berlin, Berlin, Germany
1Medical Physics Group, Institute of Diagnostic and Interventional Radiology, Jena University Hospital - Friedrich Schiller University Jena, Jena, Germany, 2Institute of Diagnostic and Interventional Radiology, Jena University Hospital - Friedrich Schiller University Jena, Jena, Germany, 3Julius Wolff Institute, Berlin Institute of Health at Charité - Universitätsmedizin Berlin, Berlin, Germany
Synopsis
An MRI-safe device guiding knee motion/loading with a rotary encoder was used during MRI measurements of multiple knee flexion-extension cycles using radial gradient echo imaging with the golden-angle as a radial increment. Reproducibility of knee motion was investigated and anatomical CINE images were reconstructed for different knee angles by synchronizing the encoder data with the MRI data and selective gating, enabling evaluation of musculoskeletal conditions.
Introduction
Conventional musculoskeletal MRI is performed in static and unloaded configurations that do not represent the dynamic physiology of joints. However, it is relevant to evaluate musculoskeletal joint conditions in the context of motion as deviations from normality can be involved in degenerative changes1. Two requirements must be met for morphological and compositional evaluation of knee tissues in the context of motion: (i) an MRI-safe device that allows guided and loaded motion within the scanner bore and (ii) reconstruction efforts such as CINE that allow for high-resolution imaging during joint motion and loading that are physiologically relevant. Here, we present a solution to both challenges for high-resolution 2D imaging during knee motion and loading.Methods
The developed device is positioned inside the MR scanner, half supported by the inner railings that guide the patient table and half by the patient table (Figure 1). Inside the bore, the device allows for up to ~40° of knee flexion. A fiber optic position sensor that measures the absolute angular position with a resolution of 0.025° is attached to the device. MRI measurements were performed on five healthy volunteers (age 22–29 years) using a clinical 3T Siemens Prisma fit scanner.To investigate reproducibility, transverse slices of the knee through the femur were acquired for each volunteer. Acquisition parameters were: 144x144 matrix, 210x21x2.5mm3 field of view, 1.5x1.5x4.8mm3 spatial resolution, 10° flip angle, 2.4ms echo time, 5.1ms repetition time, 200 repetitions with an acquisition duration of 3:51 minutes. Real-time images were reconstructed from 28 flexion-extension cycles actively performed by the subjects. A region of interest (ROI) of the femur was drawn for the first frame, and copied and translated to the remaining 27 frames such that it fit the femur (Figure 2). The ROI shift in the x- and y-directions was determined based on the position of the center of mass of the ROIs.
For CINE reconstruction, a single 2D sagittal slice of the knee was acquired using 65 repetitions of a radial golden-angle FLASH sequence2 with acquisition parameters: 320x320 matrix size, 210x210x2.5mm3 field of view, 0.66x0.66x3mm3 spatial resolution, 10° flip angle, 2.4ms echo time, 7.0ms repetition time with a total acquisition duration of 3:48 minutes. During measurements, subjects were positioned supine and secured in the device with the knee flexion-extension axis aligned with the sagittal plane. Subjects performed flexion-extension cycles under loaded conditions (13kg) to the beat of a metronome (7.5 cycles/minute). Synchronization of the knee motion with the MRI data was performed by simultaneously acquiring per repetition sequence triggers with the rotary encoder data. Based on this information, respective knee flexion angles could be ascribed to individual readouts. For retrospective CINE reconstruction, readouts were binned into knee flexion angle windows with a width of 2°, for example, the CINE image for 22° of knee flexion was constructed from all readouts acquired between 21° and 23°. Images were reconstructed using only readouts from either flexion or extension due to physiological differences in tissue morphology/morphometry between concentric and eccentric contractions.
For comparison, real-time and CINE images were reconstructed for four different angular positions with a 2° window. To examine the effects of the selected window, CINE images were reconstructed with eight different window widths for the same angular position.
Results
Figure 2 depicts the x- and y- leg translation from repeated motion relative to the first frame. Figure 3 shows the real-time and CINE reconstructed images for 4 knee angles. While the real-time images suffered from streaking artifacts and blurring, the CINE images appeared visually sharper and did not appear to suffer significantly from artifacts. Figure 4 displays CINE images for eight different angle windows, where images with a smaller window appeared to suffer from undersampling artifacts (streaking and blurring) in addition to noise, and images with a larger window appeared blurry due to poor knee angle precision. Table 1 shows that the smallest window sampled 24% of k-space and that k-space was fully sampled at windows of 3° or more.Discussion and Conclusion
Dynamic MRI measurements of the knee using an MRI-safe device for guided motion and mechanical loading with a rotary encoder enabled CINE reconstruction of images with the potential of morphological and compositional evaluation of knee tissues. For CINE reconstruction, it is important to carefully select the angle window, as small windows can lead to undersampling artifacts and loss of SNR whereas larger windows can lead to blurring from motion. Overall, image resolution and sharpness were improved compared to previous work3. While a smaller angle window was advantageous for obtaining sharp images best suited for morphological evaluation, a larger angle window could reduce measurement time by increasing the SNR - ultimately leading to a trade-off between greater knee angle precision and a larger number of readouts for reconstruction. Due to the golden-angle radial acquisition, this trade-off can be adapted solely during image reconstruction. The flexion-extension speed of 7.5 cycles/minute was slower compared to speeds typically reported4; further research should focus on acquiring faster knee motions (e.g., ~30 cycles/minute), analogous to physiological motion in everyday life such as walkingAcknowledgements
This work was supported by the German Research Foundation (DFG - Deutsche Forschungsgemeinschaft, DU 298/25-1, RE 1123/22-1). Additional support is acknowledged from the Competence Center for Interdisciplinary Prevention (KIP - Kompetenzzentrum für Interdisziplinäre Prävention) at the Friedrich Schiller University Jena and the German Professional Association for the Food and Hospitality Industry (BGN - Berufsgenossenschaft Nahrungsmittel und Gastgewerbe).References
- Andriacchi T, Mündermann A, Smith, R et al. A Framework for the in Vivo Pathomechanics of Osteoarthritis at the Knee. Annals of Biomedical Engineering. 2004;32(3):447–457.
- Krämer M, Herrmann KH, Biermann J, Reichenbach JR. Retrospective reconstruction of cardiac cine images from golden-ratio radial MRI using one-dimensional navigators. J Magn Reson Imaging. 2014 Aug;40(2):413-22
- Borotikar B, Sipprell W, Wible Е, Sheehan F. A methodology to accurately quantify patellofemoral cartilage contact kinematics by combining 3D image shape registration and cine-PC MRI velocity data. Journal of Biomechanics. 2012;45(6):1117-1122
- Sheehan F, Zajac F, Drace J. Using cine phase contrast magnetic resonance imaging to non-invasively study in vivo knee dynamics. Journal of Biomechanics. 1997;31(1):21-26
Figures
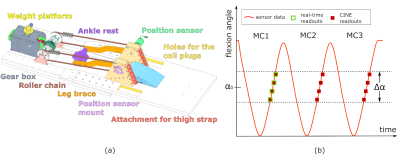
Figure 1. Depiction of the device with labeled components (a). Additional load can be added to the device/leg, allowing for more physiological conditions. The gear system translates knee motion to the platform via a roller chain. (b) Readout for a specified angular position α0 and angle window Δα during knee flexion-extension for 3 motion cycles (MC). Only the points outlined in green would be used for real-time reconstruction, while all points in red would be used for CINE reconstruction.
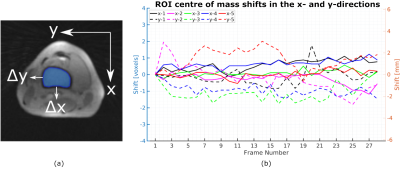
Figure 2. Real-time reconstructed image
from a transverse slice through the femur with a drawn ROI (a). Once the ROI is
copied to another frame and aligned with the femur, the ROI center of mass will
have a shift of Δx and Δy in the x- and y-directions, respectively. This
shift can be seen in (b) for 5 different volunteer scans. The mean (standard
deviation) of the shifts across all measurements was 0.3 voxels (0.5mm) for the
x- (solid lines) and 0.6 voxels (0.9mm) for the y-direction (dashed lines).
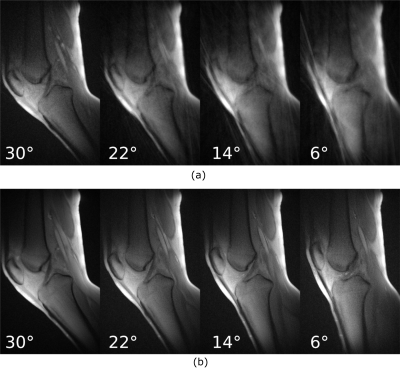
Figure 3. Real-time (a) and CINE
(b) images reconstructed for 4 different angular positions with a 2° angle
window. The images in (a) were reconstructed from readouts during the first MC,
and inconsistencies in the knee motion such as speed and range of motion can
result in some images suffering from less undersampling artefacts than others.
The images in (b) are reconstructed from multiple MCs and are visually more
consistent.
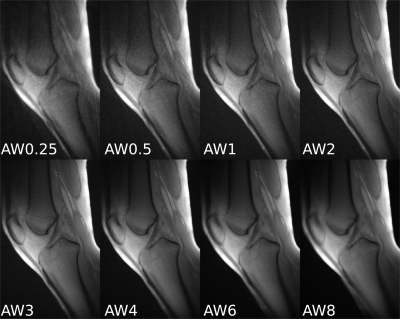
Figure 4. CINE images
reconstructed for 8 different angle windows (AW). The number of readouts with
unique orientations in k-space and the percentage of k-space sampling are shown
in Table 1.
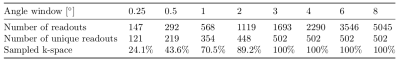
Table 1. Number of unique readouts and percentage of
k-space sampling for the CINE images shown in Figure 4.
DOI: https://doi.org/10.58530/2022/0381